By Kristina Campbell, science and medical writer
Even on the days when you don’t eat a large meal of Boston baked beans, the inside of your intestines is a gas-generating factory. This serves a valuable purpose for the body when everything is working as it should, with gases being produced and eliminated through a complex set of physiological processes. But sometimes gas becomes a problem—and this is when it’s valuable to know not only what contributes to intestinal gas symptoms, but also how dietary adjustments can alleviate some of the problems.
Dr. Fernando Azpiroz, Chief of Gastrointestinal Research at the Vall d’Hebron Research Institute and Professor of Medicine, Autonomous University of Barcelona (Spain), is an expert in both the pathophysiology of the gas produced in the digestive tract and the clinical problems related to intestinal gas. Dr. Azpiroz is the author of a chapter on intestinal gas in the well-known textbook, Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, which is now in its 10th edition. And for more than 20 years he has been conducting research on digestive tract function, intestinal gas, and the contributions of the gut microbiota.
ISAPP caught up with Dr. Azpiroz to ask him about everything you wanted to know—where intestinal gas comes from, when it becomes a problem, and the latest research on the dietary changes that can reduce symptoms of intestinal gas while keeping the gut microbiota intact.

In different parts of the digestive tract, where does intestinal gas come from?
For the most part, the gas in the digestive system comes from metabolic activities of the colonic microbiota.
In addition, some air enters the stomach during swallowing. Most of this air is eliminated by eructation (i.e. burping), so there is a homeostasis. There is a small air chamber in the stomach of about 20 mLs, and this is pure atmospheric air, or CO2 after recent consumption of carbonated drinks.
In the small intestine, the neutralization of acids and alkali can theoretically produce large amounts of CO2. However, it’s more in theory than measured in experimental conditions.
Other gases originate from the metabolism of the gut microbiota. The residues of the diet that are not absorbed in the small bowel pass into the colon. These are the parts of the diets that we, as humans, cannot use. These pass into the colon, and in the colon serve as substrates for colonic microbiota. Gas is produced during this process of colonic fermentation.
What types of gases are produced in the digestive tract?
The composition of intestinal gas depends on where in the gut it is produced.
In the stomach, the gas is virtually all atmospheric air or CO2.
In the small bowel, theoretically it should be CO2, although the hard data are very scarce.
And in the colon, the largest component is likely hydrogen and CO2. But the data on that are very limited, and it is not known for sure that these theories are really true. The measurements of gas composition, in the colon or even in the gas eliminated per anus are still uncertain but so far the main concept is that most of the gas is hydrogen and CO2, and methane in subjects that have a methanogenic microbiota.
How does this gas normally get eliminated?
Throughout the GI tract, particularly the colon, about 80% of the gases produced are absorbed through the mucosa, pass into the blood, and are eliminated by breath. So only about 20-25% of the volume of gases produced, particularly in the colon, are eliminated per anus.
What influences the amount of gas produced?
The amount of gas produced in different subjects depends on two factors: one is the diet—the amount of residues (i.e. fiber) in the diet—and the second is the type of microbiota, which is very individual. It varies a lot from one subject to another.
How much intestinal gas is ‘too much’?
From the point of view of patients, of symptoms, what might be relevant is the volume of gases produced, and possibly the type of gases. One evolving idea is that some gases, which are produced in very small quantities, might serve as neurotransmitters, might play a role, but so far the information we have about the role of these gases is very limited so we cannot extrapolate that to clinical use.
Very recent data indicate that symptoms occur when the GI tract has a poor tolerance to its contents, and particularly to gas.
So what is the factor that makes gas produce symptoms? Well there are two factors. One is the amount of gas, and the other one is the tolerance of the subject.
In healthy subjects, it will typically take a large amount of gas to develop symptoms, if at all.
But even small amounts of gas in patients that have a hypersensitivity of the gut and poor tolerance to contents might contribute to their symptoms. This can be seen because, if we reduce the amount of flatulogenic substances in their diet, the symptoms reduce.
This is if we just take into consideration the volume of gas produced, but there is also another factor.
If we give a high flatulogenic diet or a high-residue diet, we know, because we have measured, that we increase the volume of gas produced into the colon. However, we also increase the amount of the fecal content in the colon. So it could be that these diets produce symptoms because they increase the amount of gas, but also because other non-gaseous components, the fecal content of the colon, also are poorly tolerated.
How can someone manipulate their diet to change the amount of intestinal gas that’s produced?
A ‘challenge’ diet, or a high flatulogenic diet in healthy subjects, makes them sick. They go from being symptom-free to having some symptoms, particularly flatulence and bloating.
In patients, the effect of the diet is more accentuated. If patients consume a diet with high residues they get very symptomatic, and if these patients will reduce residues in the diet, they see quite an improvement.
What are the options for dietary change when someone has IBS or wants to reduce gas symptoms?
One thing that has been shown recently is that the effect of a low-residue diet is similar regardless of the type of diet. In the past ten years or so there’s been a major trend with the use of low-FODMAP fermentable oligo-, di-, mono-saccharides and polyols diets.
However, the effect of these complex diets is not better than the effect of any sensible and simple low-residue diet. So if you reduce legumes, veggies from the diet, and fruits, you get a similar improvement.
The problem with low-residue diets, in particular the low-FODMAP diet, is that they introduce a restriction of the substrates for the feeding of the microbiota, and this is deleterious to the microbiota. The microbiota is impoverished.
The other limitation of low-residue diet is that the moment that the patient returns to a normal diet, the symptoms come back.
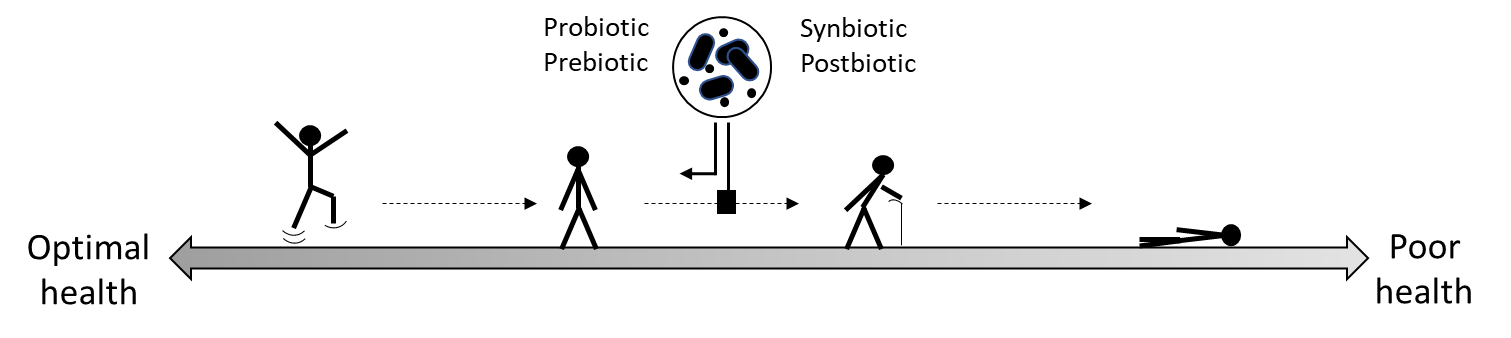
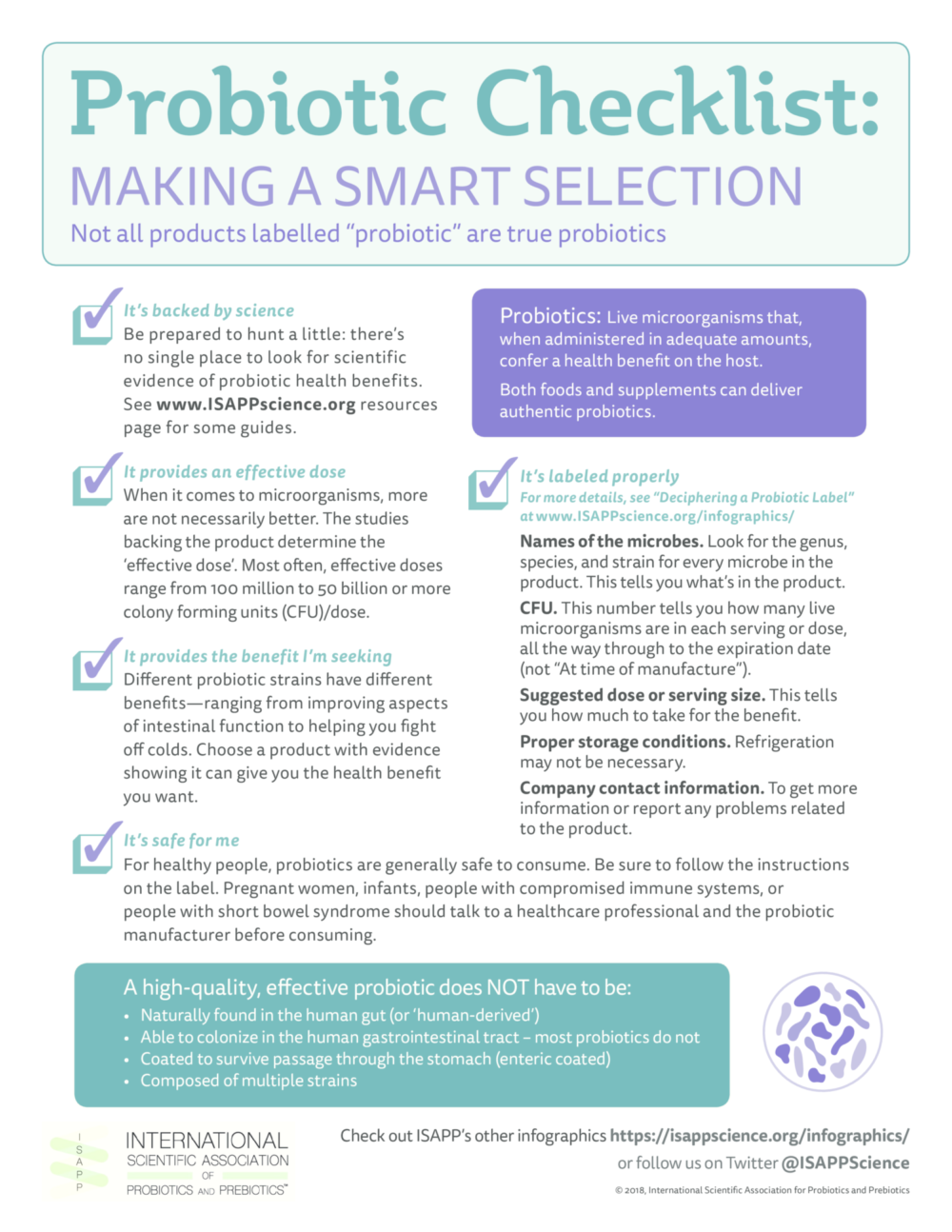
There is an alternative that has been shown in the past few years, which is to use some type of prebiotics that initially—because they are fermented—produce symptoms, but after a few days they induce an adaptation of the microbiota towards a microbiota that produces less gas with normal fermentation. And down the road, these prebiotics have a positive effect on symptoms in patients. As a matter of fact, the effect on symptoms is similar to a restrictive diet. The advantage of the prebiotics is that, after interruption, …the effect is sustained at least over a few weeks. And this is because it has been shown that prebiotics serve as substrates for microbiota and induce a proliferation of beneficial organisms.
There is also some preliminary evidence that some probiotics reduce the volume of gas production and reduce digestive symptoms in patients.
Is it a good idea to test your gut microbiota when you have IBS or gas symptoms?
There are different companies that claim that by analyzing microbiota they can diagnose some functional conditions, for instance IBS. The practical application of this technology has not been demonstrated. Usually they are expensive techniques and of no value.
It’s important to understand the real value of these methodologies and take the myth out of ‘wonder’ techniques that make a diagnosis from the microbiota and claim it explains everything.
Hopefully, this might be true in the future, but not right now. And actually many of the technologies that are used for this type of analysis are suboptimal.
A previous blog post by Dr. Bob Hutkins on diet, gut microbiota, and intestinal gas is ISAPP’s most-read blog post of all time. Read it here.