Should everyone take a probiotic? Assessment of evidence of probiotics for healthy people
By Prof. Daniel Merenstein MD and Dr. Mary Ellen Sanders PhD
During the ISAPP 2024 meeting, an article titled, “Is there evidence to support probiotic use for healthy people?” was published. The authors concluded, “…we did not find a high level of evidence to support recommendations for other endpoints we reviewed for healthy people. Although evidence for some indications is suggestive of preventive benefits of probiotics, additional research is needed.”
Those in the probiotic field are used to headlines critical of probiotics meant to sensationalize rather than accurately reflect the evidence. But this article takes a careful look at if probiotics should be used by everyone regardless of indication.
Scientific grounding for the paper
This article is an ISAPP output derived from an ISAPP 2023 discussion group that included academic and industry scientists, including the nine authors. The discussion group aimed to examine the evidence that probiotics are beneficial to healthy people at a population recommendation level.
We assembled probiotic and evidence-based medicine experts to review the literature. We chose preventative indications that we felt had some compelling evidence that healthy people would benefit from probiotics. Thus, we examined the evidence that probiotics could reduce urinary, vaginal, gastrointestinal, and respiratory infections, reduce antibiotic use, and improve risk factors associated with cardiovascular health. Populations included certain groups of individuals, including generally healthy people, those at risk for recurrent urinary and vaginal infections, and children taking antibiotics. We considered that the evidence was too nascent for this exercise for endpoints such as cognitive function, athletic performance, and dental health, and therefore did not review these endpoints.
The challenges of studying prevention
We undertook this effort to address the common question, “Should everyone take a probiotic?” In fact, there are few recommendations for any intervention for people free of underlying disease. Such interventions must have sufficient evidence of benefit and of relatively little to no risk of harm.
In raising this question for probiotics, we took inspiration from the approach of an organization tasked with evaluating preventive evidence: the United States Preventive Services Task Force (USPSTF). Since an important component of a USPSTF review is potential for harm, it is important to note here that experts considering the safety of probiotics recently concluded that commonly used probiotic strains are safe for use in the general population.
The USPSTF recognizes that preventive measures are difficult and expensive to study. Healthy populations are difficult to define and not uniformly defined across studies. The physiology of healthy people recruited into a study is generally unlikely to change, especially over the short term. So efficacy studies must either be long-term or must identify more accessible endpoints, such as validated biomarkers of disease or reduction of infectious disease, as targets for prevention. Further, the threshold of evidence for recommending any intervention to a healthy population has to be very high, partially due to the potential risk of harm. In a patient with an illness, a risk of harm may be tolerable if the benefit outweighs the risk. But in an asymptomatic individual this threshold is more difficult to determine.
It is noteworthy that some preventive measures are widely believed by the general public to be effective, but upon scrutiny of the data have been found to lack supporting evidence. For example, for healthy adults younger than 75 years of age, the Endocrine Society recently recommended against Vitamin D supplementation above the current RDA. The USPSTF has concluded that there is insufficient evidence to recommend a daily multivitamin for the prevention of cancer or cardiovascular disease, to screen for skin cancer, or to screen for speech and language delay disorders in children 5 years or younger or eating disorders in adolescents. Even diet and exercise counseling for the prevention of cardiovascular risk in healthy people received only a level C recommendation. As one would expect for recommendations for healthy people, the USPSTF imposes a high bar for required evidence. This group of experts aimed to apply a similar high bar for evidence on probiotic indications.
Meeting the strict criteria for an effective preventative measure
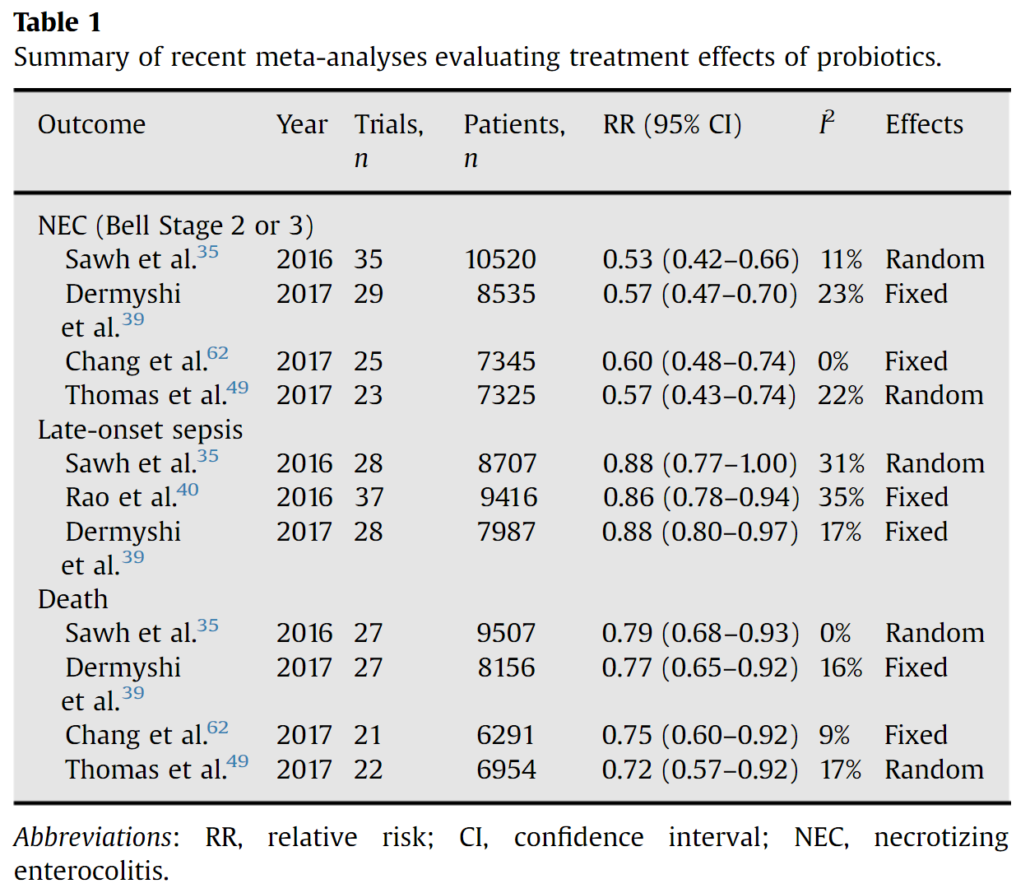
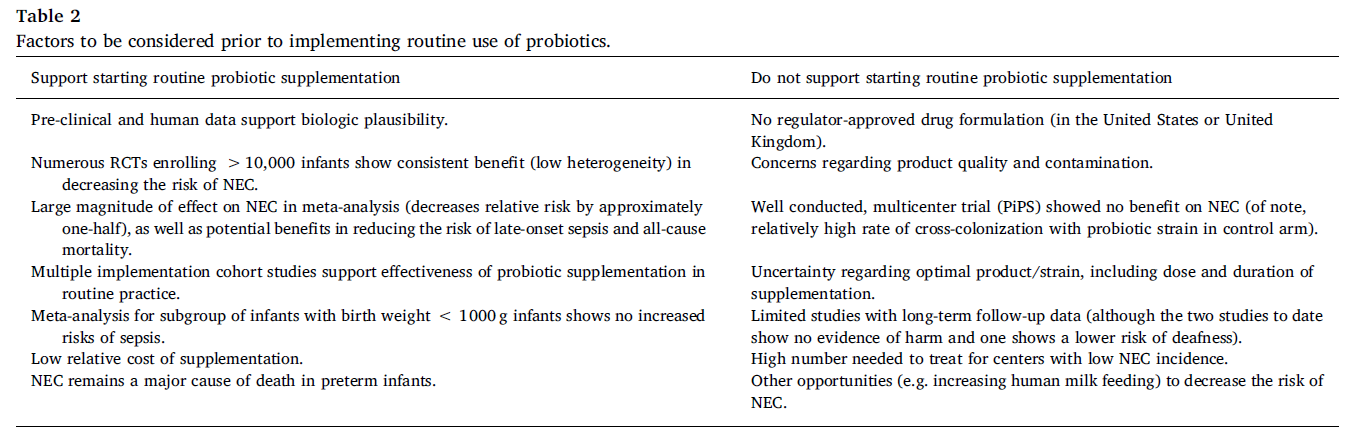
We reviewed data for indications where there were compelling studies on essentially healthy individuals showing some benefit from probiotics. But we wanted to determine if it was plausible that this body of evidence would meet a USPSTF-level of evidence for a recommendation for all healthy people. We recognized that there is sufficient evidence of efficacy to consider using specific probiotics for some indications for certain people. For example, evidence reviews have found that certain probiotics can be effective to prevent necrotizing entercolitis, reduce incidence of antibiotic associated diarrhea, reduce crying time in breast-fed colicky infants, improve therapeutic effectiveness of antibiotics to treat bacterial vaginosis, reduce risk for Clostridioides difficile infections, treat acute pediatric diarrhea, and manage symptoms of constipation. However:
Sufficient evidence of benefit to support the recommendation that “everyone should take a probiotic” is not yet available.
At ISAPP 2024 (held July 9-11), we heard from experts about the promise of probiotics for our skin as we age, for social anxiety, for immune function in children and for helping undernourished kids thrive. Those who understand the evidence level for probiotics recognize the proven and potential role for probiotics in health. Our paper does not change that. There is evidence for many individuals to take daily probiotics due to conditions they have. Interestingly, after our discussion group, the FDA approved a qualified health claim that can be used on yogurt. The claim relates to the impact of yogurt on the risk of developing diabetes. Allowed language for this claim includes:
- “Eating yogurt regularly, at least 2 cups (3 servings) per week, may reduce the risk of type 2 diabetes. FDA has concluded that there is limited information supporting this claim.”
- “Eating yogurt regularly, at least 2 cups (3 servings) per week, may reduce the risk of type 2 diabetes according to limited scientific evidence.”
This claim relied on evidence of correlative associations in humans. For our analysis, we required a higher level of evidence from randomized, controlled trials. Further, this claim applies to yogurts that may or may not contain added probiotics in addition to the yogurt starter cultures. However, it is an important preventative endpoint and supports the idea that healthy people may benefit from probiotic-containing foods.
Evidence to date suggests that with additional investment in well-designed research, the future may see probiotics reach the high standard of evidence needed for preventative recommendations in healthy people.
Further Reading
Do probiotics really benefit healthy people? from NewsMedical