Five points to know about biotics for animals, from an ISAPP-led paper
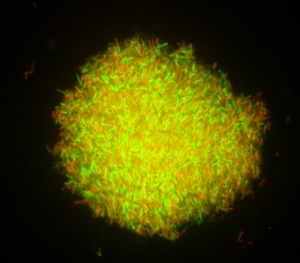
Biotics, including probiotics and prebiotics, are well known for their human health benefits. But a growing number of studies have focused on biotic use in both agricultural and companion animals. Biotics have been employed in animals to achieve a variety of health benefits as well as improvements in growth and production efficiency.
A group of animal health experts, comprising academic and industry member scientists convening at the 2023 ISAPP annual meeting, reviewed the evidence on biotics for animals, outlining what’s known to date and the likely future directions in this scientific field. Led by Prof. Kelly Swanson PhD and Emeritus Prof. George Fahey PhD, the group recently published a review in Journal of Animal Science that summarizes their discussion.
Here are five main points from their paper:
Biotic effects are likely specific to each type of animal and its living conditions
The authors caution that a biotics study on one type of animal doesn’t necessarily translate to another type of animal. They write, “Knowledge of the host species of interest is important, as differences in anatomy, physiology and microbiota populations, dietary requirements, environmental exposures, and disease susceptibility dictate biotic type and dosage.”
In addition, many studies even within the same animal species find that biotics can be variable in effectiveness. The authors note that biotics may work differently depending on the diet of the animal, its gut microbiome, or living environment, and studies should be planned with relevant applications in mind.
More work is needed to find out the most effective probiotics for companion animals
In companion animals such as dogs and cats, prebiotics are commonly used and effective whereas probiotics studied so far are less effective for addressing gastrointestinal symptoms. The primary aims of using probiotics in companion animals are to maintain overall health and improve longevity, and while some probiotic strains have shown promise for outcomes related to immunity, stress management, and metabolic health, for example, more work is needed to identify the appropriate strains and doses. The paper authors say host-adapted strains that work more effectively within the gastrointestinal tract of the animal may be identified in the future and result in better outcomes.
Probiotics have potential to greatly reduce the use of antimicrobials in agricultural animals
Traditionally, antimicrobials have been used in agricultural animals such as poultry and ruminants to prevent or treat infections, and to a lesser extent to promote growth. However, concerns about antimicrobial resistance are bringing increased attention to antimicrobial alternatives. Studies exist that show the potential of probiotics to reduce antimicrobial use in swine, poultry, and ruminants as well as aquaculture.
Co-author Shalome Bassett says, “Probiotics, as well as prebiotics, have been shown to be particularly effective in ruminants, not only through improved immunity but also increased productivity and food quality. And, importantly, there’s no evidence of residue issues with their use so dairy or meat products remain safe and nutritious.”
Shaping the animal gut microbiota in early life appears important for health
In animals as in humans, early life is an important time for establishing a gut microbiota that supports health throughout the remainder of the lifespan. Studies in multiple animal species have shown the importance of the gut microbiota for shaping early immune responses, indicating that richer microbial exposures in early life may lead to better resistance against pathogens and better overall health later in the animal’s life.
Biotic use in animals may impact human health, too
The authors say that using biotics in animals can help address challenges beyond health of the animals themselves. Using probiotics and other biotics in animals also has potential to impact human health as well. Although biotics may not have the same magnitude of effects as antimicrobials, administering probiotics to agricultural animals, for example, may be able to improve food safety by reducing zoonotic infections and antimicrobial resistance overall.
The benefits of biotic use in animals are becoming increasingly clear, both for animals and for humans who share their environment. However, each animal is unique, and the most effective biotic solutions will likely be specific to each species. As knowledge of biotic use in animals continues to expand, scientists will continue to zero in on the most effective biotic types and doses for each application.
Read the paper here.
See ISAPP’s infographic Prebiotics and Probiotics for Pets here.