ISAPP’s 2019 annual meeting in Antwerp, Belgium: Directions in probiotic & prebiotic innovation
Kristina Campbell, Microbiome science writer, Victoria, British Columbia
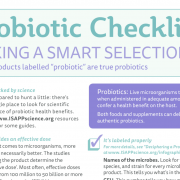
We live in a time when a simple Google search for ‘probiotics’ produces over 56.8 million hits; a time when almost everyone has heard of probiotics through one channel or another, and when an ever-increasing variety of probiotic and prebiotic products is available in different regions of the world.
The next five to ten years will be telling: will probiotics and prebiotics join the ranks of other trendy health products that experienced a wave of popularity before something else took their place? Or will they be recognized as important contributors to health through the lifespan, and establish a permanent position in the clinical armamentarium?
According to the global group of 175 academic and industry scientists who met for the ISAPP annual meeting in Antwerp (Belgium) May 14-16, 2019, one thing above all is necessary for the world to recognize the significance of probiotics and prebiotics for health: scientific innovation. Not only are technological capabilities advancing quickly, but also, new products are being evaluated by better-educated consumers who demand more transparency about the health benefits of their probiotics and prebiotics.
Participants in the ISAPP conference came together to talk about some of the leading innovations in the world of probiotics and prebiotics. Here are three of the broad themes that emerged:
Better health through the gut-brain axis
Gut-brain axis research is rapidly growing, with many investigators in search of probiotic and prebiotic substances capable of modulating brain function in meaningful ways. Phil Burnett of Oxford (UK) presented on “Prebiotics, brain function and stress: To what extent will prebiotics replace or complement drug therapy for mental health?”. Burnett approached the challenge by administering prebiotics to healthy adults and giving them a battery of psychological tests; in one experiment he found people who consumed a prebiotic (versus placebo) showed benefits that included reduced salivary cortisol and positively altered emotional bias. For those with diagnosed brain disorders, Burnett concludes from the available data that prebiotics have potential anxiolytic and pro-cognitive effects in these populations, and that prebiotics may eventually be used to complement the established treatments for some mental disorders.
Short-chain fatty acids (SCFAs) are of interest as potential modulators of brain function, but so far very little research has been carried out in this area. Kristin Verbeke of Leuven (Belgium) gave a talk entitled “Short-chain fatty acids as mediators of human health”, which covered the extent to which interventions with fermentable carbohydrates can alter systemic SCFA concentrations (rather than gut SCFA concentrations)—since the former are more relevant to effects on the brain.
Also, a students and fellows feature talk by Caitlin Cowan of Cork (Ireland) explored a role for the microbiota in psychological effects of early stress. She spoke on the topic “A probiotic formulation reverses the effects of maternal separation on neural circuits underpinning fear expression and extinction in infant rats”.
A clear definition of synbiotics
Immediately before the main ISAPP meeting, a group of experts met to propose a consensus definition of ‘synbiotic’, with the objective of clarifying for stakeholders a scientifically valid approach for the use of the increasingly-popular term. A key point of discussion was whether the probiotic and prebiotic substances that make up a synbiotic are complementary or synergistic. And if the two substances have already been tested separately, must they be tested in combination to give evidence of their health effect? The group’s conclusions, which will undoubtedly steer the direction of future R&D programs, will be published in a forthcoming article in Nature Reviews Gastroenterology & Hepatology.
Probiotics and prebiotics for pediatric populations
Probiotics and prebiotics have been studied for their health benefits in pediatric populations for many years, but in this area scientists appear to have a renewed interest in exploring new solutions. Maria Carmen Collado of Valencia (Spain) covered “Probiotic use at conception and during gestation”, explaining some of the most promising directions for improving infant health through maternal consumption of probiotics.
In recent years, technical advancements have made possible the large-scale production of some human milk oligosaccharides (HMOs); it is now an option to administer them to infants. Evelyn Jantscher-Krenn of Graz (Austria) presented a novel perspective on HMOs, with “HMOs in pregnancy: Roles for maternal and infant health”, giving a broad overview of the many ways in which HMOs might signal health status and how they might be fine-tuned throughout a woman’s pregnancy.
A discussion group on “prebiotic applications in children”, chaired by Dr. Michael Cabana of San Francisco (USA) and Gigi Veereman of Brussels (Belgium), discussed evidence-based uses of prebiotics in children in three areas: (1) prevention of chronic disease; (2) treatment of disease; and (3) growth and development. While the latter category has the best support at present (specifically for bone development, calcium absorption, and stool softening), the other two areas may be ripe for more research and innovation. The chairs are preparing a review that covers the outcomes of this discussion group.
Next year in Banff
ISAPP’s next annual meeting is open to scientists from its member companies and will be held on June 2-4, 2020 in Banff, Canada.
Photo by http://benvandenbroecke.be/