1-10 of 10 results
-

Insights into healthy aging: A story as told by gut microbiome (and other) metabolites
Metabolites, including those derived from the gut microbiome, offer a window into the complex biology of aging. They reflect not just how we live, but how well our bodies are adapting to the passage of time. -
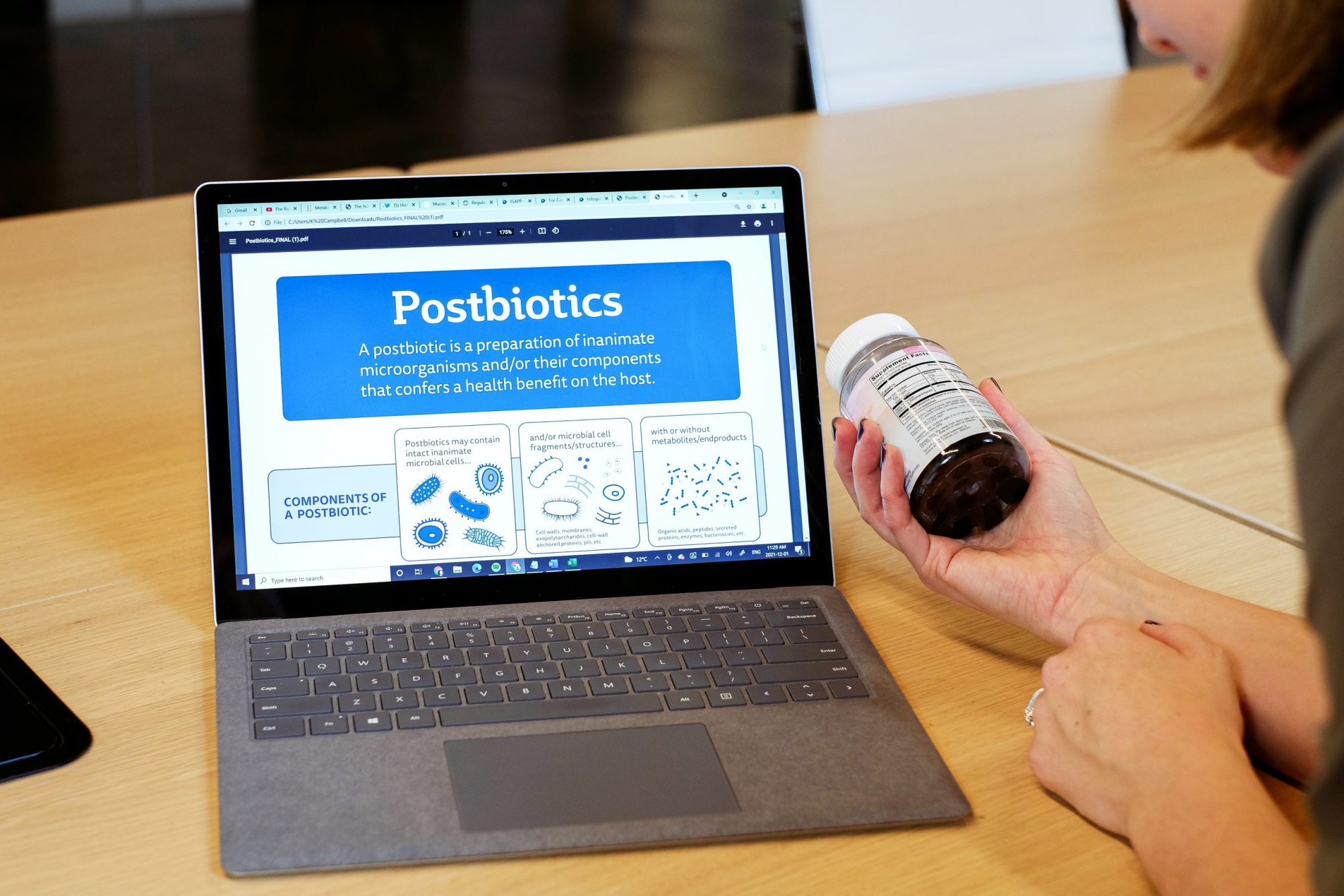
Postbiotics: A global perspective on regulatory progress
By Dr. Gabriel Vinderola PhD, CONICET, National University of Litoral, Argentina While the conceptualisation of postbiotics varies among scientists, some… -

Clarifying the role of metabolites in the postbiotic definition
By Dr. Gabriel Vinderola PhD, Instituto de Lactología Industrial (CONICET-UNL), Faculty of Chemical Engineering, National University of Litoral, Santa Fe,… -

Postbiotics: debate continues and the ISAPP definition gains support
By Dr. Gabriel Vinderola PhD, Instituto de Lactología Industrial (CONICET-UNL), Santa Fe, Argentina The publication of a new definition for… -

Can we use fermented foods to modulate the human immune system?
By Dr. Paul Gill PhD, Monash University Fermented foods have grown in popularity in recent years, marketed for their purported… -
How metabolites help us to understand the effect of gut microbes on health
By Dr. Anisha Wijeyesekera, University of Reading, UK Much literature relating to the gut microbiota has focused on microbial composition… -

Bifidobacteria in the infant gut use human milk oligosaccharides: how does this lead to health benefits?
By Martin Frederik Laursen, Technical University of Denmark, 2022 co-recipient of Glenn Gibson Early Career Research Prize Breast milk is… -

Do polyphenols qualify as prebiotics? The latest scientific perspectives
When the ISAPP scientific consensus definition of ‘prebiotic’ was published in 2017, the co-authors on the paper included polyphenols as… -

Behind the publication: Understanding ISAPP’s new scientific consensus definition of postbiotics
A key characteristic of a probiotic is that it remains alive at the time of consumption. Yet scientists have known… -

New publication co-authored by ISAPP board members gives an overview of probiotics, prebiotics, synbiotics, and postbiotics in infant formula
For meeting the nutritional needs of infants and supporting early development, human milk is the ideal food—and this is reflected…