ISAPP provides guidance on use of probiotics and prebiotics in time of COVID-19
By ISAPP board of directors
Summary: No probiotics or prebiotics have been shown to prevent or treat COVID-19 or inhibit the growth of SARSCoV-2. We recommend placebo-controlled trials be conducted, which have been undertaken by some research groups. If being used in clinical practice in advance of such evidence, we recommend a registry be organized to collect data on interventions and outcomes.
Many people active in the probiotic and prebiotic fields have been approached regarding their recommendations for using these interventions in an attempt to prevent or treat COVID-19. Here, the ISAPP board of directors provides some basic facts on this topic.
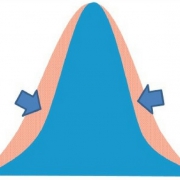
What is known. Some human trials have shown that specific probiotics can reduce the incidence and duration of common upper respiratory tract infections, especially in children (Hao et al. 2015; Luoto et al. 2014), but also with some evidence for adults (King et al. 2014) and nursing home residents (Van Puyenbroeck et al. 2012; Wang et al. 2018). However, not all evidence is of high quality and more trials are needed to confirm these findings, as well as determine the optimal strain(s), dosing regimens, time and duration of intervention. Further, we do not know how relevant these studies are for COVID-19, as the outcomes are for probiotic impact on upper respiratory tract infections, whereas COVID-19 is also a lower respiratory tract infection and inflammatory disease.
There is less information on the use of prebiotics for addressing respiratory issues than there is for probiotics, as they are used mainly to improve gut health. However, there is evidence supporting the use of galactans and fructans in infant formulae to reduce upper respiratory infections (Shahramian et al. 2018; Arslanoglu et al. 2008). A meta-analysis of synbiotics also showed promise in repressing respiratory infections (Chan et al. 2020).
Mechanistic underpinnings. Is there scientific evidence to suggest that probiotics or prebiotics could impact SARS-CoV-2? Data are very limited. Some laboratory studies have suggested that certain probiotics have anti-viral effects including against other forms of coronavirus (Chai et al. 2013). Other studies indicate the potential to interfere with the main host receptor of the SARS-CoV-2 virus, the angiotensin converting enzyme 2 (ACE2). For example, during milk fermentation, some lactobacilli have been shown to release peptides with high affinity for ACE (Li et al. 2019). Recently, Paenibacillus bacteria were shown to naturally produce carboxypeptidases homologous to ACE2 in structure and function (Minato et al. 2020). In mice, intranasal inoculation of Limosilactobacillus reuteri (formerly Lactobacillus reuteri) F275 (ATCC 23272) has been shown to have protective effects against lethal infection from a pneumonia virus of mice (PVM) (Garcia-Crespo et al. 2013). These data point towards immunomodulatory effects involving rapid, transient neutrophil recruitment in association with proinflammatory mediators but not Th1 cytokines. A recent study demonstrated that TLR4 signaling was crucial for the effects of preventive intranasal treatment with probiotic Lacticaseibacillus rhamnosus (formerly Lactobacillus rhamnosus) GG in a neonatal mouse model of influenza infection (Kumova et al., 2019). Whether these or other immunomodulatory effects, following local or oral administration, could be relevant to SARS-CoV-2 infections in humans is at present not known.
Our immune systems have evolved to respond to continual exposure to live microbes. Belkaid and Hand (2016) state: “The microbiota plays a fundamental role on the induction, training, and function of the host immune system. In return, the immune system has largely evolved as a means to maintain the symbiotic relationship of the host with these highly diverse and evolving microbes.” This suggests a mechanism whereby exposure to dietary microbes, including probiotics, could positively impact immune function (Sugimura et al. 2015; Jespersen et al. 2015).

The role of the gut in COVID-19. Many COVID-19 patients present with gastrointestinal symptoms and also suffer from sepsis that may originate in the gut. This could be an important element in the development and outcome of the disease. Though results from studies vary, it is evident that gastrointestinal symptoms, loss of taste, and diarrhea, in particular, can be features of the infection and may occur in the absence of overt respiratory symptoms. There is a suggestion that gastrointestinal symptoms are associated with a more severe disease course. Angiotensin converting enzyme 2 and virus nucleocapsid protein have been detected in gastrointestinal epithelial cells, and infectious virus particles have been isolated from feces. In some patients, viral RNA may be detectable in feces when nasopharyngeal samples are negative. The significance of these findings in terms of disease transmission is unknown but, in theory, do provide an opportunity for microbiome-modulating interventions that may have anti-viral effects (Cheung et al. 2020; Tian et al. 2020; Han et al. 2020).
A preprint (not peer reviewed) has recently been released, titled ‘Gut microbiota may underlie the predisposition of healthy individuals to COVID-19’ (Gao et al. 2020) suggesting that this could be an interesting research direction and worthy of further discussion. A review of China National Health Commission and National Administration of Traditional Chinese Medicine guidelines also suggested probiotic use, although more work on specific strains is needed (Mak et al. 2020).
Are probiotics or prebiotics safe? Currently marketed probiotics and prebiotics are available primarily as foods and food/dietary supplements, not as drugs to treat or prevent disease. Assuming they are manufactured in a manner consistent with applicable regulations, they should be safe for the generally healthy population and can be consumed during this time.
Baud et al. (in press) presented a case for probiotics and prebiotics to be part of the management of COVID-19. Although not fully aligned with ISAPP’s official position, readers may find the points made and references cited of interest.
Conclusion. We reiterate, currently no probiotics or prebiotics have been shown to prevent or treat COVID-19 or inhibit the growth of SARSCoV-2.