Can we use fermented foods to modulate the human immune system?
By Dr. Paul Gill PhD, Monash University
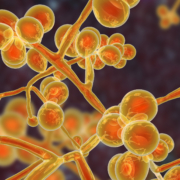
Fermented foods have grown in popularity in recent years, marketed for their purported health effects, including on the gut microbiome and immune system. Many of us have had a family member or friend recommend to us kombucha or sauerkraut based on a claim of curing their ailments. However, a reliable recommendation goes beyond anecdotal evidence and the science of how fermented foods confer any health benefits is often poorly understood. We often associate health effects of fermented foods with bacteria such as lactobacilli or Bifidobacterium, but what is lesser known is the role of microbial metabolites. These have sparked recent interest, particularly amongst researchers.
Many fermented foods naturally contain a mixture of live microorganisms and metabolites, such as phenolic compounds and short-chain fatty acids (SCFA). All of these components have the potential to impact host immunity, through two main mechanisms. Firstly, by directly interacting with local gut immune cells that have receptors for bacterial components such as lipopolysaccharide or peptidoglycan. Secondly, by modulating gut microbiota composition or function that will lead to indirect changes to host immunity. Together, these mechanisms are important for regulation of gut barrier integrity and immune homeostasis. Furthermore, bacterial metabolites such as SCFA are also absorbed by the portal vein and reach peripheral circulation, suggesting that they may also play a role in regulating systemic immune responses.
Although many of these findings are based upon observations from in vitro studies or pre-clinical models, several pilot studies in humans have also reported similar effects. A recent trial in a small cohort of healthy people found that consumption of an average of six servings of fermented foods per day for 10 weeks was associated with reduced serum inflammatory markers. Furthermore, consumption of a diet that included three servings of apple cider vinegar each day for three weeks, increased levels of plasma short-chain fatty acids and reduced subsets of circulating lymphocytes in a group of 20 healthy people. Taken together, these studies highlight the potential anti-inflammatory effects of fermented foods and postbiotics.
It remains a challenge to attribute consumption of fermented foods to alterations in host immunity, particularly due to the complex nature of these foods. This is particularly the case for traditional fermented food products that are not well characterised. After isolation and identification of individual metabolites within fermented foods, characterisation of how these compounds are absorbed and interact within the body is also necessary to determine how frequently they should be consumed to have meaningful effects on the immune system. Future studies need to be designed of sufficient duration, with a realistic dietary intervention and optimal timing of biological sampling is crucial to validate observations from exploratory trials. Finally, studies in patients with immune deficiencies will be needed to assess safety and potential therapeutic benefit. Alternatively, studies in healthy people during an immune challenge, such as during vaccination, are another desirable approach to investigate immune and therapeutic effects of fermented food consumption.
The scientific and medical communities, alongside the food industry, are continuing to improve our understanding of how fermented foods may benefit our health and immune system, including which components are responsible for any health benefits. Future studies are still needed to confirm if these may be of therapeutic benefit, and who may benefit the most from consuming these products. As our knowledge evolves, it is important that we continue to follow expert groups such as ISAPP to keep well informed and correctly communicate this information to patients and the public.