Do polyphenols qualify as prebiotics? The latest scientific perspectives
Kristina Campbell MSc, Science writer
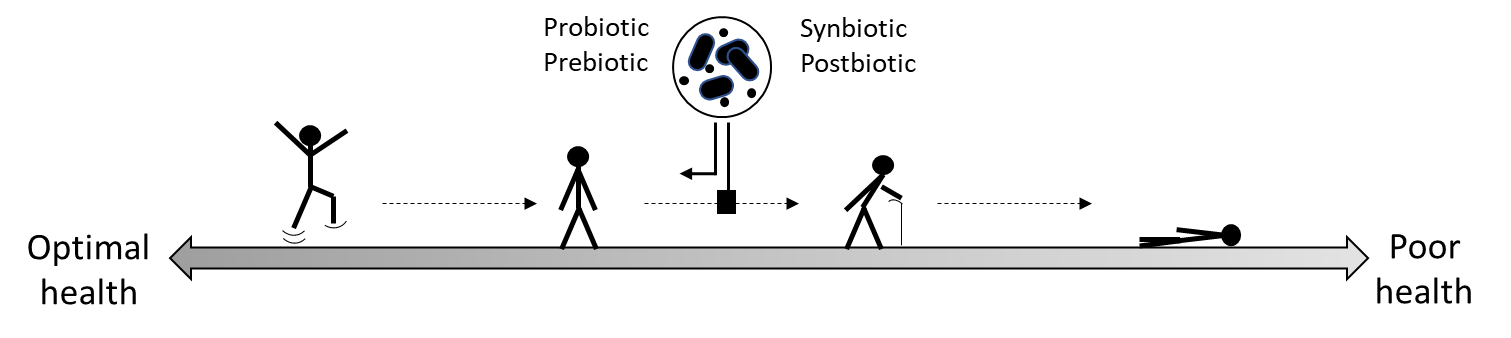
When the ISAPP scientific consensus definition of ‘prebiotic’ was published in 2017, the co-authors on the paper included polyphenols as potential prebiotic substances. At the time, the available data on the effect of polyphenols on the gut microbiota were insufficient to show a true prebiotic effect.
An ISAPP webinar held in April 2022, aimed to give an update on the health effects of polyphenols and their mechanisms of action, along with how well polyphenols fit the prebiotic definition. Prof. Daniele Del Rio from University of Parma, Italy, and Prof. Yves Desjardins from Université Laval, Canada, presented the latest perspectives in the field.
What are polyphenols?
Polyphenols are a group of compounds found in plants, with over 6000 types identified to date. They can be divided into two main categories, flavonoids and non-flavonoids.
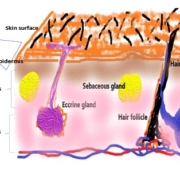
Polyphenols are absorbed in two different ways in the body. A very small fraction is absorbed in the small intestine, but 95% of them reach the lower gut and interact with gut microbiota. Although polyphenols have a special capacity to influence the activities of microorganisms, some resident microorganisms, in turn, can change the chemical structure of polyphenols through enzymatic action. These interactions produce a unique array of metabolites, which may be responsible for some of polyphenols’ prebiotic effects.
What are the health effects of polyphenols?
Epidemiological studies show that polyphenols in the diet are associated with many health benefits, including prevention of cardiovascular disease, certain cancers, and metabolic disease. These effects occur through various mechanisms. However, association is not proof of causation. So how good is the evidence that polyphenols can lead to health benefits?
Numerous human studies exist, but the most robust study to date for the health benefits of polyphenols is a randomized, controlled trial of over 20,000 adults, published in 2022, which showed supplementation with cocoa extract reduced death from cardiovascular events (although it did not reduce the number of cardiovascular events).
What are the mechanisms of action for polyphenols?
Polyphenols have multiple mechanisms of action. Del Rio focuses on the metabolites produced from dietary polyphenols called flavan-3-ols, which are found in red wine, grapes, tea, berries, chocolate and other foods. Along with colleagues, he showed that the metabolites produced in response to a polyphenol-rich food occur two ‘waves’: a small wave in the first 2 hours after ingestion, and a larger wave 5-35 hours after ingestion. The second wave is produced when flavan-3-ols reach the colon and interact with gut microbiota.
Work is ongoing to link these metabolites to specific health effects. Along these lines, Del Rio described a study showing how cranberry flavan-3-ol metabolites help defend against infectious Escherichia coli in a model system of bladder epithelial cells. These polyphenols are transformed by the gut microbiota into smaller compounds that are absorbed—so the health benefit comes not from the activity of polyphenols directly, but from the molecule(s) that the gut microbiota has produced from the polyphenols.
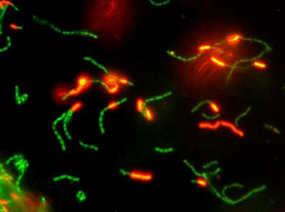
How else do polyphenols work? Ample evidence suggests polyphenols interact in different ways with gut microbes: they have direct antimicrobial effects, they affect quorum sensing, they compete with bacteria for some minerals, and/or they modify ecology, thereby affecting biofilm formation. Desjardins explained that these interactions may occur in parallel: for example, polyphenols may exert antimicrobial effects when they reach the colon, and at the same time, microorganisms in the gut begin to degrade them.
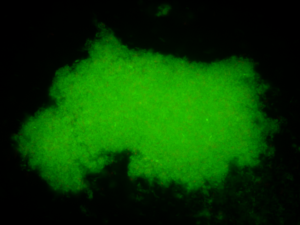
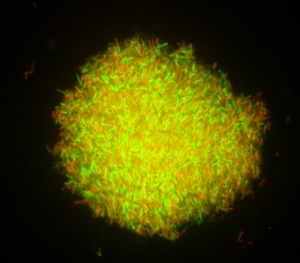
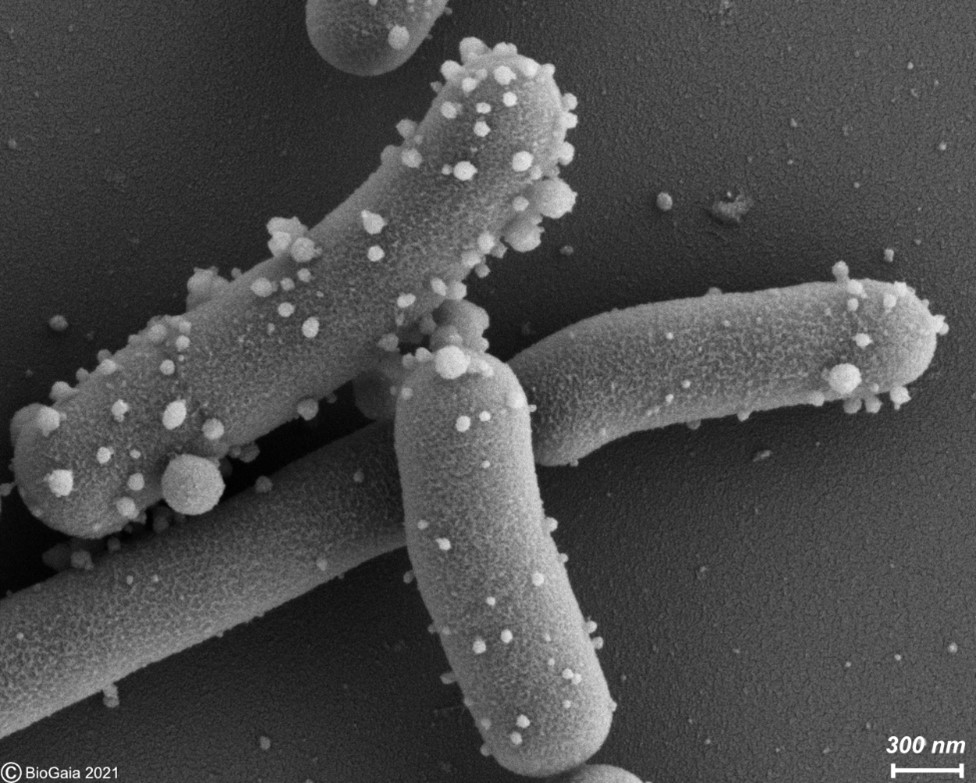
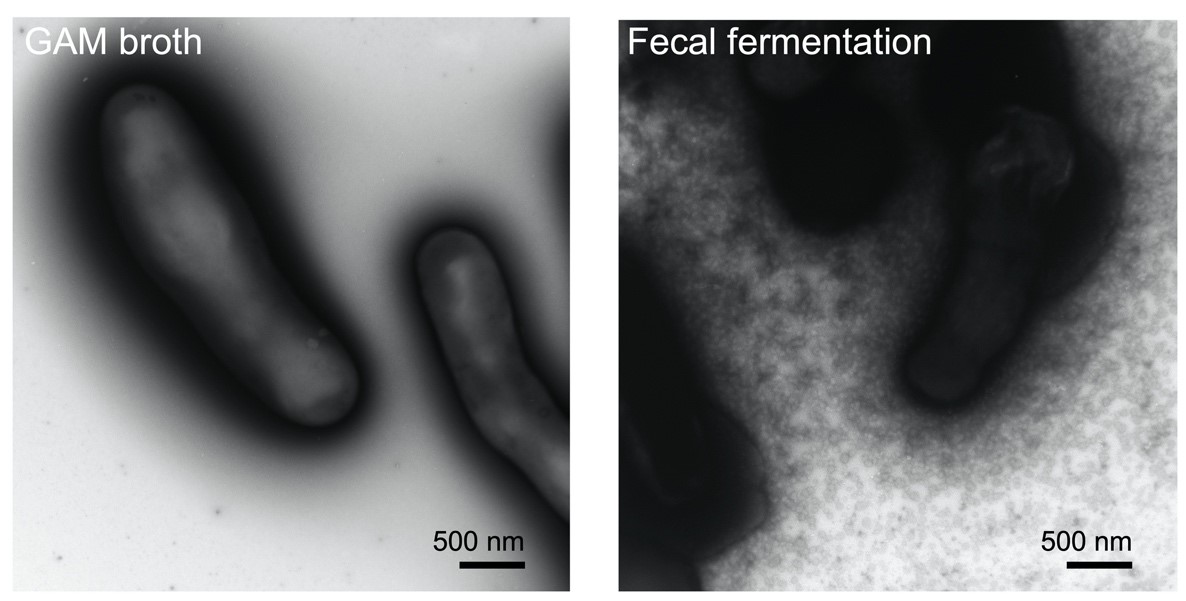
The mode of action of polyphenols Desjardins studies is the prebiotic mode of action—or as he describes it, “prebiotic with a twist”. A landmark paper from 2015 showed how cranberry polyphenols had protective effects on metabolism and obesity through the creation of mucin in the intestine, which formed a good niche for Akkermansia muciniphila, a keystone bacterial species for good metabolic health. Other polyphenols have since been shown to work the same way: by stimulating production of mucin, thereby providing ideal conditions for beneficial bacteria to grow. In this way, polyphenols appear to show small-scale effects comparable to the effects of probiotics, by inducing a host response that alters the bacterial niche.
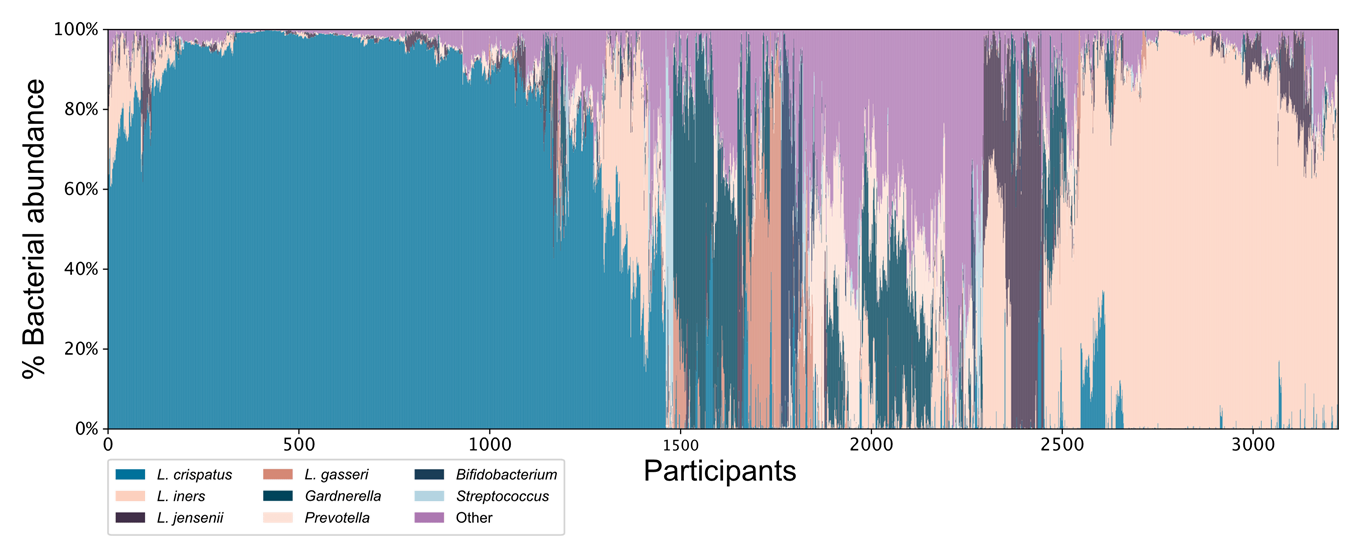
Are the effects of polyphenols individual?
Del Rio offered some evidence that the health effects of polyphenols, via metabolites, is personalized: a study showed the existence of three distinct patterns of metabolite production in response to dietary polyphenols (ellagitannins). These may depend on the particular microbes of the gut and their ability to produce the relevant metabolites—so in essence, in each case the gut microbiota is equipped to produce a certain set of metabolites in response to polyphenols. More work is needed, however, to be able to personalize polyphenol intake.
Do polyphenols qualify as prebiotic substances?
Polyphenols clearly interact with gut microbiota to influence human health. The definition of a prebiotic is “a substrate that is selectively utilized by host microorganisms conferring a health benefit”. Given the available evidence that polyphenols are not metabolized or utilized by bacteria in all cases in the same direct way as carbohydrate prebiotics, Desjardins sees them as having a “prebiotic-like effect”. Rather, polyphenols are transformed into other biologically active molecules that ultimately provide health benefits to the host. These prebiotic-like properties of polyphenols are nicely summarized in a 2021 review paper and include decreasing inflammation, increasing bacteriocins and defensins, increasing gut barrier function (thereby reducing low-grade inflammation), modulating bile acids, and increasing gut immuno-globulins.
Overall, the speakers showed that polyphenols exert their health effects in several ways—and while the gut microbiota are important for their health effects, polyphenols, as a heterogenous group, may not strictly meet the criteria for prebiotics. Clearly, more research on polyphenols may reveal other mechanisms by which these important nutrients influence the gut microbiome and contribute to host health, and they may someday be regarded as prebiotics.
Watch the replay of the ISAPP webinar here.