Microbiome endpoints in clinical trials for biotics – where do we stand and what have we learnt?
By Marla Cunningham, ISAPP Executive Director
I’m sure you’ve read the results of trials similar to these (fictional) conclusions:
‘Our findings showed an increase in Faecalibacterium and Enterococcus, two groups associated with reduced inflammation, and a decrease in Clostridium spp, which have been associated in previous studies with metabolic risk. These results suggest a beneficial modulation of the microbiome by intervention X, possibly contributing to the observed health benefits in this study.’
In biotic (and other) intervention trials, it is commonplace to see the practice of hypothesising beneficial mechanistic roles for taxonomic changes based on literature review associations. Yet despite the apparent logic of this approach, such findings are only suggestive and require confirmation in rigorous experimental studies before we can have confidence that the microbiome is indeed moving to a healthier state.
A problem that persists in the microbiome field is that confounding factors make the interpretation of microbiota changes and their implications for health challenging. Two of the key challenges are causation (both attribution and directionality) and the interindividual nature of microbiome responses:
- Cause or consequence. Changes in microbiome features during an intervention trial may be a direct result of the intervention, a result of other exposures, like dietary or lifestyle changes, or a consequence of the change in host health status. Microbiota, host and diet influence each other in an interrelated triad – change any, and the others can respond in turn (except diet doesn’t respond – or does it? Food cravings might be linked to the microbiome). While the impact of the microbiome on host health is often highlighted, the environment within the gut also influences the microbiome – with host changes in inflammatory tone, immune status and gut barrier function impacting the functions and numbers of the microbes within. Thus, the causal contribution of any microbiota change is rarely easy to disentangle.
- Interindividual responses. Microbiota composition differs widely between individuals and populations. If putatively beneficial changes are demonstrated in one population, such results may be difficult to extrapolate to other populations, limiting external validity of study findings. Further, within studies, heterogenous responses across study participants are averaged into mean group response rates, obscuring unique causes and consequences to be found within individual outcomes.
In the face of these and other challenges, what progress have we made in recent years in interpreting gut microbiome changes, and where does the science stand now on the application and interpretation of microbiome endpoints in clinical trials? Below are six areas of developing insights and continued progress in this area.
These and related questions are the subject of ISAPP’s most recent podcast series on the implementation of microbiome science in biotic science and practice. Listen here to episodes throughout May and June where ISAPP experts interview scientists on key new publications on this topic. Links and notes included below for further listening and reading.
Shift from composition to function
Through one lens, gut microbes can be seen as metabolic factories – consuming substrates and producing metabolites, orchestrated by their genetic machinery and modulated by environmental exposures. A huge amount of functional redundancy exists in any given microbiome, with shared genes and functions present across a broad range of taxa. In one individual, butyrate production may be carried out by a different set of microbes than in another – and the loss of any one taxon may be well compensated by another taking over the same niche and performing similar metabolic functions. As this understanding has grown, and shotgun sequencing prices have decreased, metagenomic data has been increasingly used for not just better taxonomic resolution, but also for readouts of functional potential based on gene abundance. Providing a readout of the butyrate-production capacity of a microbiome provides a useful tool to compare across microbiomes, and make inferences and comparisons about the host-relevant outputs produced.
However, despite recent emphasis on the promise of functional rather than compositional readouts, as well as the difficulties of interindividual and population level variability, Ghosh and colleagues recently developed a species-based health-associated core keystone (HACK) index with significant promise. Utilising a dataset of 45,000 gut microbiomes across six continents, they identified and ranked a list of 201 consistently health-associated taxa, with positive predictive value to differentiate healthy and diseased cohorts as well as responses to health-associated interventions such as the Mediterranean diet. (Listen to Prof Tarini Ghosh explain the HACK index in this episode.)
Expression rather than potential
While gene analysis provides an indication of metabolic potential, metabolomics provides direct measurement of the chemical milieu created by microbial and host interactions. A snapshot summation of the outputs of microbial activity can be taken from blood, urine, stool and other samples. Interpretation of such findings can be challenging, however, with analyses separated by various degrees of removal from microbial production – due to degradation of molecules, cross feeding metabolism, and duplicate host production. An important example is SCFA measurement. While SCFAs are understood as a key mediator of microbe:host interactions, the utility of their measurement in faeces has proved disappointing, with a lack of correlation to colonic production (in large part, because SCFA transporters are upregulated for greater utilisation when production is increased). However, plasma SCFAs can be reliable postprandial markers, providing temporally relevant information about the microbiota response to interventions (read key takeaways on SCFA measurement here). Joos and colleagues (listen to Raphaela Joos here on outputs from the Human Microbiome Action Consortium) recommend metabolomic methods as adjuncts to metagenomic sequencing approaches as key to better understanding the functional impacts of interventions.
Where to measure?
Whether culturing, gene sequencing or profiling molecules, the wealth of microbiome analysis and interpretation in the literature is limited to the most common sample type – faeces. If we were solely interested in correlations of the microbiome with rectal health, faeces would be a good sample choice – spatially and temporally relevant (albeit reflecting the luminal microbiota more than the adherent mucosal populations). However, interactions of biotic substances with the microbiota occur throughout the small and large intestine, with local microbiome profiles that differ significantly from the faecal microbiome. These discrepancies may significantly cloud our ability to accurately identify relevant causal relationships between interventions, microbial markers and health status. While sampling in more proximal locations has long been a challenge due to its invasive nature, advances have been made in ingestible sampling devices to provide data on other gastrointestinal sites, and capture changes which may be occurring in different spatial and temporal dimensions than those in faeces. The field awaits more insights from trials such as these, to reveal the potential of these new windows into biotic:microbiota:host interactions.
Who is the healthy control?
The majority of microbiota associations with health and disease have been deduced through case:control studies, where the healthy group is defined through variable inclusion/exclusion criteria, such as absence of known disease and lifestyle risk factors. The key operative factor, and challenge in this approach is that the risk factors and health status must be ‘known’ in advance. Further, in the absence of any existing host genetic or environmental risk, the microbiota of any currently healthy individual may be the latent risk factor itself, predisposing to future disease. To address this challenge, Joos and colleagues (more here) proposed large inclusive longitudinal cohorts where the definition of health emerges over time, reducing misleading conclusions because of miscategorising ‘healthy’ control groups.
Awareness of these challenges within the body of literature when interpreting microbiome readouts, and preferencing longitudinal comparison groups, may go some way towards reducing erroneous conclusions about the significance of microbiota changes.
Considering population-specific definitions of microbiome improvement
Consider two patients. One is in remission from inflammatory bowel disease, with their most important treatment goal being to prevent recurrence. Another patient has a family history of early death from cardiovascular disease, and wants to reduce their long term cardiometabolic risk. Conceivably, in each of these situations, there may be a different set of microbiota functions to optimise (and minimise), in order to promote the specific host:microbiome interactions relevant to their health goals. Could a microbiome that is well-suited to protect against one type of disease in one type of host and dietary context be ill-suited to protect against a different type of disease in a different host and context?
This possibility that a ‘health-promoting microbiome’ may look different for different patient populations, or even between individuals, may be a path forward for future research and application of biotic therapies. While ‘personalisation’ and ‘precision nutrition’ are current buzzwords in the field, this often amounts to assessing an individual’s position in comparison to an ‘optimal’ microbiota, and aiming to personalise interventions to move individuals from their respective baselines towards this healthier (microbially-defined) position. Beyond this, we might need to consider the possibility that the ideal microbiota of each population may differ, as a function of their health status, exposures and healthcare needs – creating population-specific metrics against which to assess progress.
Is microbiome analysis relevant?
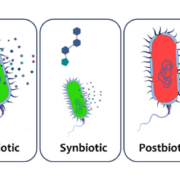
While biotics are often thought of as being microbiome-modulating strategies, all of the biotics family are known to have direct interactions with the host, e.g. via epithelial, endocrine and immune receptor interactions – with or without any contribution from the commensal microbiota. Further, excessive focus on the study of microbiota impacts may detract from the ultimate goal of any health-related intervention – to improve health – demonstrated by meaningful improvements in clinical endpoints.
Sanders and Hill reflect on some of the challenges with microbiome measures in their recent perspective article (here), and highlight key considerations for each biotic substance with regards to the relevance and utility of microbiome endpoints. For example, since prebiotics are by definition targeted at commensal microbes, measuring microbiota outcomes may be of higher relevance in prebiotic studies. Contrast this with postbiotics, which likely mediate much of their activity though proximal interactions of bioactive cellular components with host receptors, where microbiome endpoints may be exploratory at best, or other host-related mechanisms may be of greater priority to explore.
While best practice in this field remains far from clearcut, ongoing research, debate, and expert thinking continues to move us forward with important considerations and insights for a more nuanced application and interpretation of microbiome data in biotic studies.