Pasteurized Akkermansia muciniphila as a postbiotic: EFSA approval and beyond
By Prof. Seppo Salminen, University of Turku, Finland
Earlier this year, the European Food Safety Authority (EFSA) delivered an opinion that heat-treated Akkermansia muciniphila is safe for use as a novel food in the European Union. EFSA described A. muciniphila as a “well‐characterised non‐toxin producing, avirulent microorganism that has been reported as part of normal gut microbiota” and determined based on a literature review that its safety is adequate for use as a food supplement or in foods for special medical purposes, at a specified maximum dose.
ISAPP connected with three individuals from A-Mansia Biotech, the company that initiated the EFSA request: Prof. Willem M. de Vos and Prof. Patrice D. Cani, as well as the company CEO Michael Oredsson. They jointly answered some questions on their EFSA success and plans for the future.
Originally, what led you to test whether the pasteurized form of the live microbe might be able to confer a health benefit?
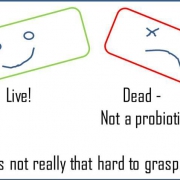
We first noticed that killing Akkermansia by using autoclaving (121°C 20°C) completely abolished the beneficial effects of Akkermansia. However, we wanted to test whether a milder procedure (i.e. pasteurization) could keep some structures of the outer membrane of Akkermansia intact and therefore still able to interact with the host. We knew that several other classical probiotics (types of lactobacilli) partly retained their effects after pasteurization. Our surprise was to see that pasteurization successfully maintained the effects of Akkermansia compared to the live form, but even increased its efficacy.
Pasteurised Akkermansia has now been extensively studied for safety and health effects. Does this make it the first real postbiotic, as defined by ISAPP?
If we are accepting the ISAPP definition proposed in 2021, we can answer yes to this question. Prof. Cani in his scientific capacity believes indeed that the product (pasteurized Akkermansia) is unique and can fall under this definition. Whether A-Mansia will be positioning the pasteurized Akkermansia as a postbiotic according to that definition is still to be discussed.
Pasteurised Akkermansia has been demonstrated to control gut barrier and reduce inflammation associated with fat storage and obesity – will we see a product that helps in weight loss/control?
Akkermansia is clearly playing a major role by tackling the gut barrier dysfunction which is the root cause of the different metabolic problems mentioned here (i.e., inflammation, fat storage, liver/fat tissue inflammation) and they are all connected to better energy expenditure/oxidation when a lower inflammation/insulin resistance is observed. Therefore, pasteurized Akkermansia should help to maintain a healthy weight and abdominal fat. A product focusing on a better weight management is currently under development at A-Mansia.
Is the next step to apply for an EU health claim?
All the current human investigations and studies at our company are aiming at fulfilling future EU health claims.
It took two years to get the acceptance for the safety of inanimate pasteurised Akkermansia – what do you think of this timeframe for safety assessment?
This is perfectly in line with what the EFSA was expecting, although it was a few months delayed with the COVID-19 crisis. The assessment was very clear, smooth and well managed by the EFSA.
In general, what do you think the future holds for postbiotics as food ingredients?
We are entering into a new era, first with next-generation beneficial bacteria, and Akkermansia as one of the most studied (if not the most studied). The pasteurized form is so active, stable, and easy to use that the postbiotic era, as led by this example, is a novel and innovative manner of targeting the microbiome for improving/maintaining health.
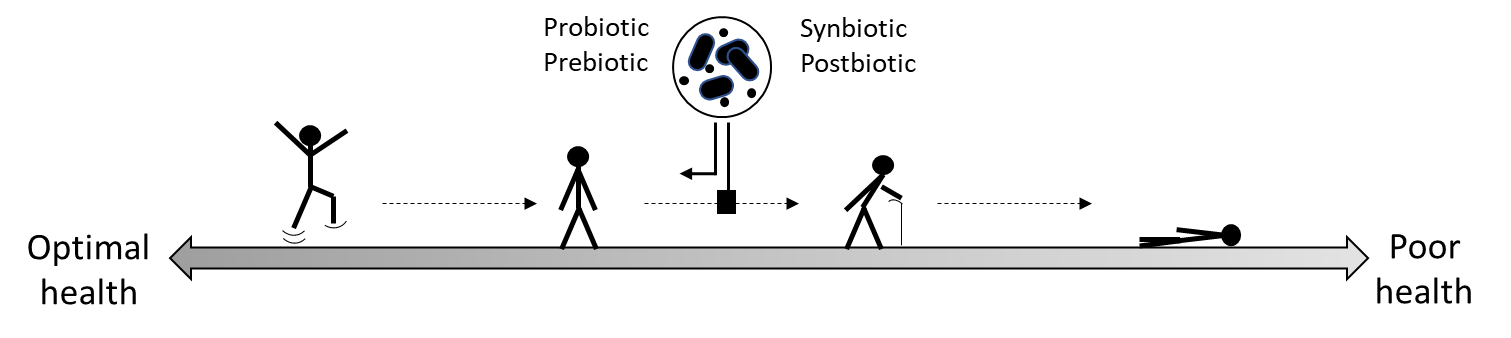
As the science on health benefits for similar postbiotic substances continues to advance, we may see more ingredients qualifying as true postbiotics. More products are likely to follow a similar path, considering the practical advantages of delivering non-living substances to consumers.