Understanding the gut microbiome in dogs and other pets, with Prof. Jan Suchodolski DACVM PhD

Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | RSS
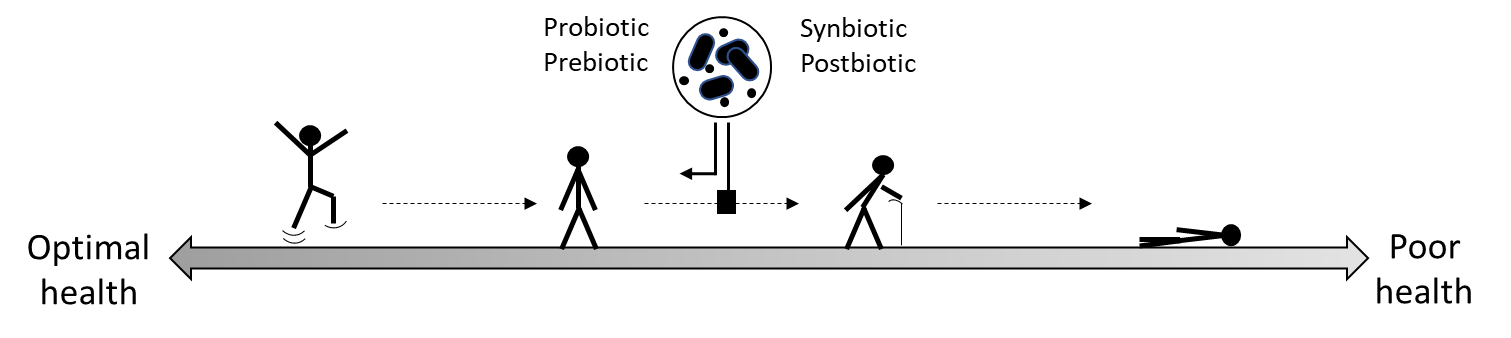
This episode features Prof. Jan Suchodolski DACVM PhD from Texas A&M University, discussing the gut microbiome in dogs and other companion animals as part of our series on the role of biotics in animal health. Prof. Suchodolski’s lab focuses on understanding gastrointestinal (GI) diseases in pets and developing diagnostic tests for research and clinical practice. His lab works on building a model of what’s happening with animal health, combining microbiome measures with measures of host health. For example, they found that severe gut microbiome dysbiosis in dogs reflected a greater extent of mucosal damage, contributing to the big picture of GI disease. Certain microbiome features when combined with metabolites are promising biomarkers of GI disease in pets. Test reproducibility is highly important, and treatment tends to be multi-modal. Prof. Suchodolski cautions against direct-to-consumer pet microbiome tests, noting that unvalidated assays are very common.
Episode abbreviations and links:
- Study showing dysbiosis with antibiotic administration in dogs: Effects of metronidazole on the fecal microbiome and metabolome in healthy dogs
- Study showing microbiome and metabolite features of dogs with inflammatory bowel disease: Alteration of the fecal microbiota and serum metabolite profiles in dogs with idiopathic inflammatory bowel disease
- Purina Institute Microbiome Forum Virtual Event 2024
Additional resources:
ISAPP infographic: Prebiotics and probiotics for pets
ISAPP blog post: Are prebiotics good for dogs and cats? An animal gut health expert explains
ISAPP blog post: Using probiotics to support digestive health for dogs
About Prof. Jan Suchodolski DACVM PhD:
Jan S. Suchodolski is a professor, Purina PetCare Endowed Chair for Microbiome Research, associate director and head of microbiome sciences at the Gastrointestinal Laboratory at Texas A&M University. He received his DrVetMed from the University Vienna, Austria and his PhD in veterinary microbiology from Texas A&M University. He is board certified in immunology by the American College of Veterinary Microbiologists (ACVM). His research is focused on developing biomarkers for gastrointestinal disease and therapeutic approaches for the modulation of the intestinal microbiota. He has authored or co-authored more than 400 peer-reviewed articles in the area of veterinary gastroenterology and microbiome research. In 2024, he received the AVMA career achievement in canine research award.