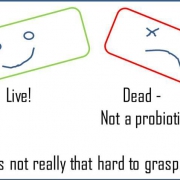
Dead bacteria – despite potential for benefit – are not probiotics
Re-posted from an original blog article by Dr. Mary Ellen Sanders, ISAPP Executive Science Officer
At the 2018 International Scientific Association of Probiotics and Prebiotics (ISAPP) meeting in Singapore, two renowned speakers reported unpublished research documenting the health benefits of dead bacteria.
Prof. Hill showed that an inactivated Lactobacillus strain reduced anxious behavior, reduced cortisol levels, and impacted the microbiome in a mouse model. Prof. Patrice Cani showed that heat-killed Akkermansia muciniphila were sufficient to ameliorate obesity and diabetes in mice. Both professors made the point that these microbial preparations were not probiotics.
Prof. Colin Hill is the lead author on the oft-cited and -downloaded (over 40,000 times) ISAPP consensus paper reaffirming the definition of probiotics, which emphasizes that probiotics must be alive when administered. This, of course, does not preclude health effects of dead bacteria. One just must remember that dead bacteria are NOT probiotics. Many different types of microbe-derived substances such as metabolites, cell wall fragments, enzymes, and neurochemicals, can have beneficial physiological effects. A 2016 review by de Almada et al. lists a couple dozen published studies of physiologically active dead bacteria.
Preserving the long-accepted definition of probiotics as ‘live microbes’ is important to the many stakeholders involved in the field. Consumers should be able to purchase a product labeled as ‘probiotic’ and know that it contains an effective level of live microbes. Regulators should know that a product without an adequate level of live microbes is fraudulent if called a probiotic. Scientists should be able to use the term and have reviewers and readers understand that they are referring to functions of live microbes. An agreed-upon definition enables us to be precise when discussing an issue. Saying that because dead bacteria have a health effect and they should be called ‘probiotics’ is like saying that because vitamin D has a health benefit, the term ‘vitamin A’ should include vitamin D.
What are implications of the fact that dead microbes may have health effects?
Stewards of the probiotic field can expect increased frustration with popular press writers. I’ll use a recent example to make this point. The June 2018 Cooking Light Magazine /Special Gut Health Issue included an article that lists sourdough bread as a top probiotic-containing fermented food. When the error about misusing the term ‘probiotic’ to describe a food that contained no live probiotic bacteria was pointed out to the editor by Jo Ann Hattner, MPH RD author of Gut Insight, Cooking Light chose to ignore advice from an expert and justify their mistake by using an irrelevant observation that both live and dead cells in probiotic products may generate beneficial biological responses. Apparently, the expertise she derived from a paper that described the “probiotic paradox” trumped the considered opinions of global expert scientists/researchers and the FAO/WHO, who agree that probiotics must be alive when administered. It’s quite a simple concept. It is true that some dead microbes may have some health benefit (although evidence of such an effect is much lower than that available from controlled human trials on actual probiotics), but they are NOT probiotics.
Confusion. Some audiences will be confused by the idea that probiotics that are killed can have health benefits. Inaccurate writers, such as the Cooking Light author above, will perpetuate this error. This is unfortunate, since the probiotic concept is a long-standing one, backed by much mechanistic and clinical evidence. Conflating probiotics with dead bacteria will lead to confusion over important aspects of an effective probiotic product.
Overages. It is not uncommon for commercial products to be formulated with live microbes at time of manufacture that far exceed the number claimed on the label. This is to assure that the product meets label claim at the end of shelf life, as probiotics often die to some extent during storage. Sometimes this ‘overage’ can reach 10-fold more than the level guaranteed on the product, although more typically it’s 2- to 5-fold. If over the course of shelf life the viable count drops to label claim, then dead microbes may comprise as much as 90% of the microbes present. We don’t know if these dead bacteria – although no longer probiotics – have physiological benefits, as no studies have been conducted on this form of inactivated cells, but it’s an interesting possibility. When we study a probiotic product, perhaps that product needs to be characterized by both the level of live and dead microbes that are present. Means of inactivation, such as heat, pressure, irradiation, or sonication, may impact the physiological activity of the resulting dead cells.
Opportunity. Keeping probiotics alive in commercial products is a challenge. Research such as Prof. Cani’s targets an expanded range of microbes – many isolated from the human GI tract – that cannot be easily grown and stabilized in commercial products. Further, these microbes lack the history of safe use that food-associated microbes have, and so administration of high numbers of these next-generation probiotics will require proof of safety. If these microbes can be killed and still deliver health benefits, the commercialization process could be simplified.
ISAPP may need to consider convening another consensus panel to address these newly emerging terms, such as postbiotic and paraprobiotic. Then we can all be on the same page when using these terms, which have important scientific, nutritional and clinical impact. Of course, even if ISAPP does this, authors may still choose to ignore it.