Ambient yogurts make a global impact
By Prof. Bob Hutkins, PhD, University of Nebraska Lincoln, USA
Quick, which country consumes the most yogurt? Must be France? Or the Netherlands? Maybe Turkey? The United States, perhaps? Try none of the above: the answer is China.
While many other countries consume way more yogurt than China on a per capita basis, China’s population gives it an advantage, with 1.4 billion potential consumers. And yogurt has become one of the most popular snack foods in China. It’s especially trendy among young and affluent urbanites. Indeed, total consumption of yogurt in China now exceeds that of France, the Netherlands, Turkey, and the United States, combined!
Whereas per capita consumption of yogurt in China in 2000 was around 1 kg per person per year, it’s now approaching 5 kg. Yogurt consumption even exceeds that of fluid milk.
Considering that dairy consumption was virtually non-existent in China for thousands of years, this trend is nothing short of a cultural phenomenon. While some of the yogurt consumed in the country is produced by domestic manufacturers, yogurt and yogurt ingredients are also being imported from other countries in the region, including New Zealand and Australia.
There is, however, one major difference between yogurt typically consumed in China and the products consumed in other regions. Indeed, ambient yogurt, short for “yogurt-based product for ambient distribution”, is all the rage in China.
Ambient yogurt and yogurt drink products, as the name implies, are stable at room temperature. This is achieved by heat-treating the yogurt after fermentation. Many ambient yogurts are aseptically processed similar to ultra-high-temperature processed (UHT) products, leaving the product commercially sterile (i.e. without live microbes) and stable for up to a year. In China, these products can still be labeled as yogurt.
Not only are these ambient yogurt products convenient for retailers, but also, a cold-chain infrastructure, often absent in rural areas of China, is not necessary during transport and distribution. Perhaps for this reason, ambient yogurts are also being introduced in other regions, including Africa, South America, and the Middle East.
The popularity of yogurt in China, in the absence of a live microbe label declaration, is evidently due to the ‘healthy’ virtues or halo effect ascribed to yogurt, because of its high protein, calcium, and vitamin content. Perhaps there are also postbiotic benefits in the yogurt – this would be an interesting topic for research. But the novel flavors, textures and grab-and-go convenience, especially for drinkable yogurt products, also appeals to teens and young adults.
Traditionalists balk at the very idea of heat-treating yogurt and inactivating the live microorganisms. In some countries, such products cannot even be labeled as yogurt. In the U.S., these products can be labeled as yogurt but must be further labeled as “heat-treated”.
In reality, consumers’ expectation of live microbes in yogurt is so ingrained that heat-treated yogurts are nearly impossible to find in the United States. Indeed, yogurt, kefir, and other cultured milk and non-dairy products are promoted, in part, on the high number of viable microbes they contain. Probiotics are added to more than 90% of the yogurts sold in the United States.
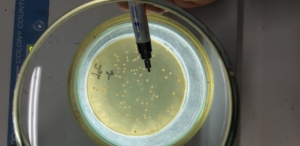
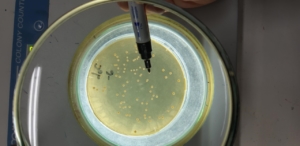
According to international CODEX standards, yogurt must be made with Lactobacillus delbrueckii subsp. bulgaricus and Streptococcus thermophilus, AND must contain at least 107 CFU/g “through to the date of minimum durability after the product has been stored under the storage conditions specified in the labeling”. Any other labeled bacteria must be present at a minimum of 106 CFU/g. The CODEX standards have been widely adopted, although some countries have lower minimum levels.
Interestingly, and despite appeals by yogurt manufacturers, the U.S. Food and Drug Administration does not require minimum numbers of CFUs for yogurt. They have been considering changes that would be consistent with CODEX for more than a decade. In regions that do not require the CODEX standards, the International Dairy Foods Association offers the Live & Active Cultures (LAC) seal, which requires 107 CFU/g of yogurt cultures at time of manufacture.
The China National Food Safety Standard for Fermented Foods does specify a minimum Lactobacillus count of 106 CFU/g, but importantly, also includes the following footnote:
“products that have gone through heat treatment after the fermentation process will not be subjected to any requirements on the minimum Lactobacillus Count”
Such products, however, must be labeled as heat-treated. It should be noted that there is still a substantial market for more traditional (chilled) yogurt containing live microorganisms. Still, ambient yogurts account for most of the yogurt consumed in China.
Given the relatively flat yogurt market in Europe and the United States, it should not be surprising that this rapidly growing market in China has attracted so much attention. The China Nutrition Society and government policymakers have recommended that consumers increase dairy consumption to 3 times higher than current levels. That means a lot more yogurt will be consumed in China.
Translated, that means, from culture companies to processing and packaging industries, there will continue to be plenty of interest, innovation, and investment in yogurt for the Chinese population. For example, new generation yogurt products have recently been introduced with the claim of having 90 days’ shelf-life and containing live probiotic bacteria.
Still, whether by new or traditional technologies, the availability and consumption of live microbes in yogurt and other cultured products may be expected to increase as Chinese consumers become more informed about their health benefits. Perhaps, as cold-chain infrastructure also improves, these live yogurts may become a bigger part of the yogurt culture in China.







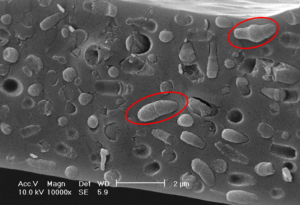
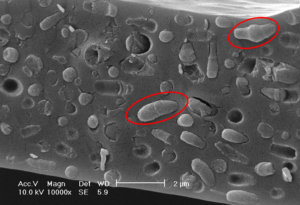


 Thanks to Metchnikoff, research on Bulgaria and Bulgarian yogurt was put on the map because of our healthy way of living and eating fermented foods. You may know this part of the story. Still, few actually know that Metchnikoff was intrigued by the work of the Bulgarian researcher Stamen Grigorov a few years earlier. In fact, it was because of Stamen Grigorov’s work that we now know ‘who’ (i.e. which microbes) live in our yogurt and how essential those tiny bacteria are. In 1905 Stamen Grigorov actually discovered and isolated for the first time Lactobacillus bulgaricus (now known as Lactobacillus delbrueckii subsp. bulgaricus) from homemade yogurt. That’s why we are so proud of Bulgarian yogurt. Not only do we love to eat it, but the probiotic research was partially initiated in our country, and an entire Lactobacillus species is named after our country. There is even a small museum dedicated to Bulgarian yogurt and to the work of Stamen Grigorov, located in the house where he was born. In the museum, if you are visiting Bulgaria, you can learn how to make yogurt at home and a bit more about the history of Grigorov’s discoveries.
Thanks to Metchnikoff, research on Bulgaria and Bulgarian yogurt was put on the map because of our healthy way of living and eating fermented foods. You may know this part of the story. Still, few actually know that Metchnikoff was intrigued by the work of the Bulgarian researcher Stamen Grigorov a few years earlier. In fact, it was because of Stamen Grigorov’s work that we now know ‘who’ (i.e. which microbes) live in our yogurt and how essential those tiny bacteria are. In 1905 Stamen Grigorov actually discovered and isolated for the first time Lactobacillus bulgaricus (now known as Lactobacillus delbrueckii subsp. bulgaricus) from homemade yogurt. That’s why we are so proud of Bulgarian yogurt. Not only do we love to eat it, but the probiotic research was partially initiated in our country, and an entire Lactobacillus species is named after our country. There is even a small museum dedicated to Bulgarian yogurt and to the work of Stamen Grigorov, located in the house where he was born. In the museum, if you are visiting Bulgaria, you can learn how to make yogurt at home and a bit more about the history of Grigorov’s discoveries. But honestly, nothing is the same as the homemade yogurt. Many people still make yogurt at home, including my father. I don’t quite remember a time when there was no homemade yogurt on the table at home. It was initially my grandmother making the yogurt and the white Bulgarian cheese (it is nothing to do with Feta but that’s the closest way to explain what it is). So it was somehow logical that my father started making yogurt as well. He knows the technique from his grandmother and grew up with fresh homemade yogurt. My grandparents had a lot of cows, sheep, and goats, so we always had plenty of milk to ferment. Making yogurt at home is so very simple that more and more young people dare to do it. In fact, making yogurt is so easy, I wonder why I am not doing it myself during the lockdown.
But honestly, nothing is the same as the homemade yogurt. Many people still make yogurt at home, including my father. I don’t quite remember a time when there was no homemade yogurt on the table at home. It was initially my grandmother making the yogurt and the white Bulgarian cheese (it is nothing to do with Feta but that’s the closest way to explain what it is). So it was somehow logical that my father started making yogurt as well. He knows the technique from his grandmother and grew up with fresh homemade yogurt. My grandparents had a lot of cows, sheep, and goats, so we always had plenty of milk to ferment. Making yogurt at home is so very simple that more and more young people dare to do it. In fact, making yogurt is so easy, I wonder why I am not doing it myself during the lockdown.