Do fermented foods contain probiotics?
By Prof. Maria Marco, PhD, Department of Food Science & Technology, University of California, Davis
We frequently hear that “fermented foods are rich in beneficial probiotics.” But is this actually true? Do fermented foods contain probiotics?
The quick answer to this question is no – fermented foods are generally not sources of probiotics. Despite the popular assertion to the contrary, very few fermented foods contain microbes that fit the criteria to be called probiotic. But this fact does not mean that fermented foods are bad for you. To uphold the intent of the word probiotic and to explain how fermented foods actually are healthy, we need to find better ways to describe the benefits of fermented foods.
Probiotics are living microorganisms, that when administered in adequate amounts, confer a health benefit on the host (Hill et al 2014 Nat Rev Gastroenterol Hepatol). This current definition reflects minor updates to a definition offered by an expert consultation of scientists in 2001 convened by the Food and Agriculture Organization of the United Nations (FAO) and the World Health Organization. Evident from the definition, a microbial strain is not a probiotic unless a health benefit has been found with its use. At a minimum, the strain should be proven to be beneficial in at least one randomized controlled trial (RCT). Probiotics must also be defined at the strain level through genome sequencing (a strain is a single genotype of a species).
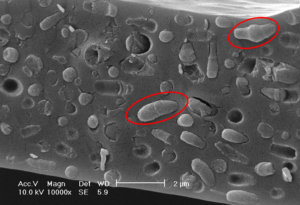
Fermented foods, on the other hand, have no requirement to improve health. Fermented foods are foods and beverages made through desired microbial growth and enzymatic conversion of food components. This definition was recently formulated by an ISAPP consensus panel of scientific experts to affirm the common properties of all foods of this type and to differentiate foods that may look or taste similar but are not made using microbes (Marco et al 2021 Nat Rev Gastroenterol Hepatol). Fermented foods encompass an expansive variety of foods made from animal and plant sourced ingredients and produced from all types of microbial metabolism. The desired characteristics of these foods are frequently how they look, smell, and taste. There no expectation in this definition that fermented foods alter health in any way.
There is also no requirement for fermented foods contain living microbes at the time they are ingested. Foods such as bread, chocolate, and beer are fermented but then are baked, roasted, and/or filtered. This means those fermented foods cannot be probiotic.
Some fermented foods, such as kimchi and kombucha, are typically eaten with living microbes present. However, the microbes in those foods usually do not meet the criteria to be called probiotic. Whether the fermented food was made at home or purchased from the supermarket, studies investigating whether the microbes in those fermented foods are specifically responsible for a health benefit remain to be done. Those foods also do not contain microbes defined to the strain level, nor is the number of living microbes typically known. An exception to this is if specific strains previously shown to provide a health benefit in one or more RCT are intentionally used in the production of the food and remain viable at expected numbers over the shelf-life of that fermented food product. An example of this would be a commercial fermented yogurt that has an added probiotic strain remaining viable at the time of consumption, beyond the strains that carried out the fermentation.
Despite these distinctions between probiotics an fermented foods, the probiotics term has pervaded common lexicon to mean “beneficial microbes”. In contrast to pathogenic or harmful microbes, beneficial microbes are those that are understood to help rather than hurt bodily functions. However, just as we do not assume that all pathogens cause the same disease or result in the same severity of symptoms, we should also not expect that beneficial microbes all serve the same purpose. By analogy, automobiles are useful vehicles which help us to get from place to place. We do not expect that all automobiles perform like those used for Formula 1 racing. Microbes are needed to make fermented foods and may be beneficial for us, but we should not assume that those drive health benefits like established probiotic strains.
What are the consequences of calling fermented foods probiotic when they include undefined numbers of living microbes for which strain identities are not known? One can suppose that there is no harm in labeling or describing those products as “probiotic” or “containing probiotics”. However, by doing so, confusion and misunderstanding is created and too often, spread by journalists, nutritionists, scientists, and medical professionals. For example, news articles in reputable sources have written that foods like kefir, kimchi, sauerkraut made from beets or cabbage, pickles, cottage cheese, olives, bread and chocolate are rich in probiotics. As misuse perpetuates, what becomes of bona fide probiotics shown with rigorous study to benefit health, such as reducing the incidence and duration of diarrhea or respiratory infections? It becomes difficult to know which strains have scientific proof of benefit. Just as there are laws for standards of food identity, we should strive to do the same when describing microbes in fermented foods.
Avoiding the term probiotic when describing fermented foods should not stop us from espousing the myriad of positive attributes of those foods. Besides their favorable sensory qualities, fermented foods are frequently safer and better tolerated in the digestive tract than the foods they are made from. During the production of fermented foods, microbes remove or reduce toxins in the ingredients and produce bioactive compounds that persist long after the microbes that make them are gone.
Even though the living microbes in fermented foods may not rise to the standard of a probiotic, they may provide health benefits. We just don’t have the studies to prove that they do. With more study, we may find that viable microbes in fermented foods work similarly to probiotics in the digestive tract through shared mechanisms. This is already known for yogurts. Yogurt cultures share the ability to deliver lactase to the intestine, thereby improving tolerance of lactose by intolerant individuals. Clinical and epidemiological studies performed on fermented foods already suggest an association between them and different health benefits but as we recently explained (Marco et al 2021 J Nutrition), more work is needed in order to understand if and what benefits these microbes provide.
For now, we should simply continue enjoying the making and eating of fermented foods and reserve the term probiotics for those specific microbial strains which have been shown to improve our health. Marketers should resist labeling products as containing probiotics if their products do not meet the criteria for a probiotic. Indeed, the descriptor “live and active cultures” more accurately reflects the microbial composition of many fermented foods, and should be used until controlled human trials demonstrating health benefits are conducted.
Additional resources:
How are probiotic foods and fermented foods different? ISAPP infographic.
Fermented foods. ISAPP infographic.
What are fermented foods? ISAPP video.
Are fermented foods probiotics? Webinar by Mary Ellen Sanders, PhD.