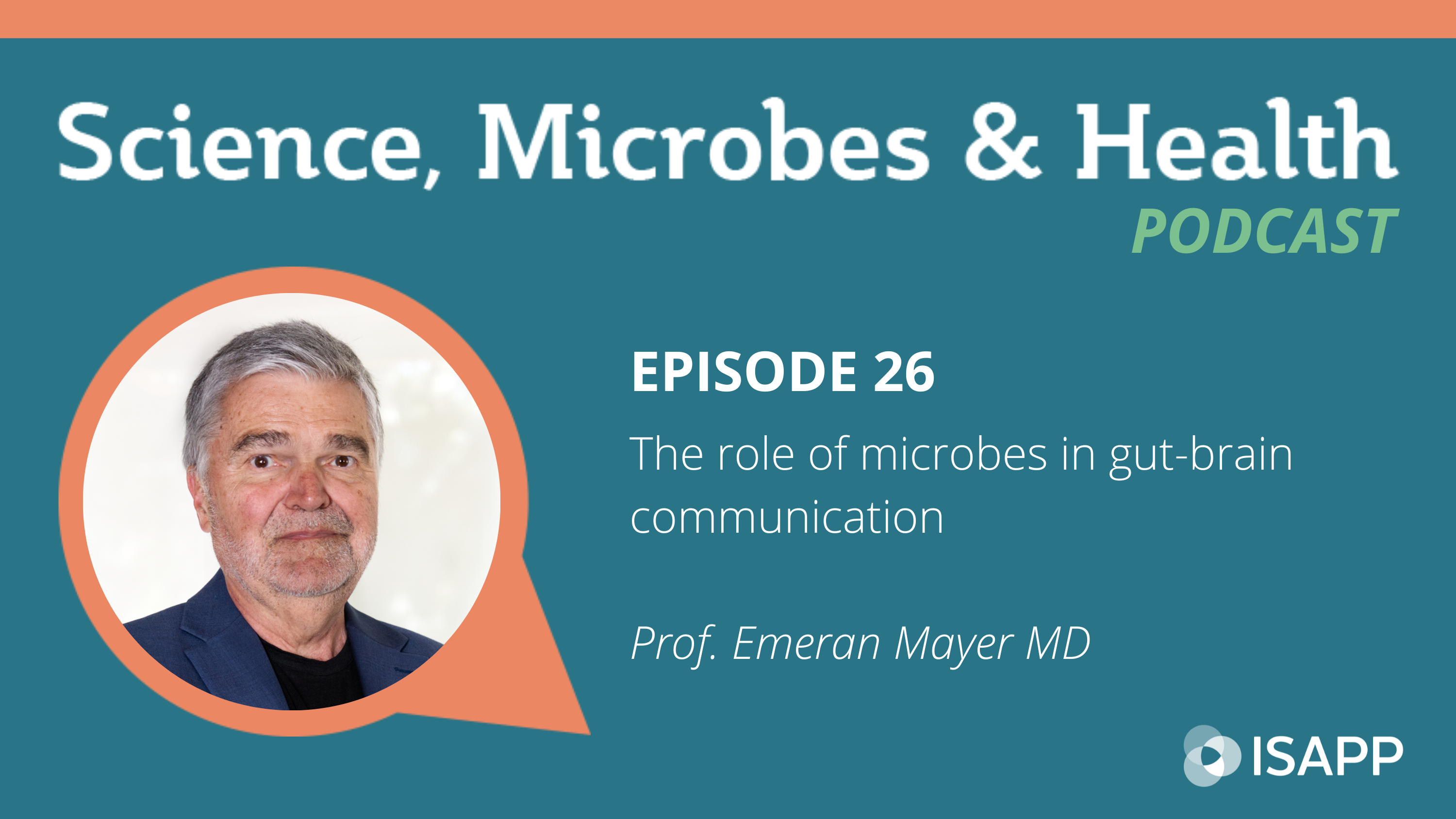
Archive Highlight: The role of microbes in gut-brain communication, with Prof. Emeran Mayer MD

Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | RSS
Continuing our series on the microbiota-gut-brain axis, we are highlighting Episode 26 from our archives. In this episode, ISAPP podcast host Prof. Dan Tancredi PhD welcomes guest Prof. Emeran Mayer MD, a gastroenterologist and researcher at University of California Los Angeles. They talk about the microbiota-gut-brain axis, covering its evolutionary origins and how this complex system works in the human body to support overall health.
Key topics from this episode:
- Microbiota-gut-brain communication has a long evolutionary history: microbes have been around for billions of years and they stored a lot of information in their genes. At some point in evolution microbes got inside the digestive tube of a primitive marine animal called hydra and it proved advantageous for this animal.
- The hydra shows the origin of the human enteric nervous system (ENS): microbes live inside this tube and transfer genes to the nerve cells of this digestive tube, showing the origin of neurotransmitters.
- Today in humans the neurotransmitters influence gene expression of microbes and change the microbial behaviors; the metabolites produced feed back to the brain.
- Prof. Mayer’s initial interest as a gastroenterologist was the ENS and how it regulates motility. Subsequently the ENS was found to regulate many gut functions. The gut also houses a large part of the immune system and a complex hormonal system, and all these systems are connected with each other and communicate with the brain.
- There is an increasing understanding that many chronic diseases relate to Inappropriate engagement of the immune system, starting in the gut.
- When Prof. Mayer started in the field, the term “gut health” did not exist. Now it’s a ubiquitous term which has associations with wellbeing, acknowledging the gut has influence on many other body systems.
- The associations between gut (microbiota) and brain health started with provocative animal experiments from Cork, Ireland, in which researchers manipulated the gut microbiome and found changes in emotion-like behaviors of animals. However, it has been difficult to translate to human interventions.
- How do microbiome-targeted dietary interventions affect the brain? We do know the “Standard American Diet” (deficient in fiber) has changed the gut microbes in a way that compromises the production and maintenance of the gut barrier.
- There are many misconceptions about “leaky gut”, but basically contact between beneficial microbes and immune system sensors stimulate the immune system of the gut to low-grade inflammation. This can alter the tight junctions, making the gut more permeable, and ultimately this can affect the brain. Diet can affect the role of microbes in maintaining an effective gut barrier.
- Prof. Mayer describes how he ended up studying the microbiota-gut-brain axis – he would not have predicted how important and popular this field would become.
- In the future, there will be more sophisticated and personalized interventions. He sees a paradigm shift happening from reductionist approaches in medicine to systems biological approaches. This field is making us acknowledge that diet will play a major role.
Episode links:
- Prof. Mayer’s first academic book, Basic and Clinical Aspects of Chronic Abdominal Pain (Pain Research and Clinical Management)
- Prof. Mayer’s first book for the general public, The Mind-Gut Connection
- Review on microbiota-gut-brain axis: The Microbiota-Gut-Brain Axis: From Motility to Mood
- Review on the impact of diet on intestinal permeability: Influence of a high-fat diet on gut microbiota, intestinal permeability and metabolic endotoxaemia
- Review on microbiota-dependent interactions between diet and the immune system: Human nutrition, the gut microbiome, and immune system: envisioning the future
About Prof. Emeran Mayer MD:
Emeran A Mayer is a Gastroenterologist, Neuroscientist and Distinguished Research Professor in the Department of Medicine at the David Geffen School of Medicine at UCLA, the Executive Director of the G. Oppenheimer Center for Neurobiology of Stress & Resilience and Founding Director of the Goodman Luskin Microbiome Center at UCLA. He is one of the pioneers and leading researchers in the bidirectional communication within the brain gut microbiome system with wide-ranging applications in intestinal and brain disorders. He has published 415 scientific papers, co edited 3 books and has an h-index of 125. He published the best selling books The Mind Gut Connection in 2016, the Gut Immune Connection in June 2021, and the recipe book Interconnected Plates in 2023. He is currently working on a MasterClass and a PBS documentary about the mind gut immune connection. He is the recipient of numerous awards, including the 2016 David McLean award from the American Psychosomatic Society and the 2017 Ismar Boas Medal from the German Society of Gastroenterology and Metabolic Disease.