1-8 of 8 results
-

Can Probiotics Prevent Respiratory Tract Infections in Infants and Children?
Imagine you are a primary care pediatrician practicing in an area where respiratory tract infections (RTIs) are particularly common during… -

Can we use fermented foods to modulate the human immune system?
By Dr. Paul Gill PhD, Monash University Fermented foods have grown in popularity in recent years, marketed for their purported… -

Shaping microbial exposures and the immune system in childhood: Can sandboxes be probiotic?
By Prof. Seppo Salminen, University of Turku, Finland Gut microbiota researchers have established that microbial exposures in early life can… -

Why researchers need to understand more about the small intestinal microbiome
By Prof. Eamonn M. M. Quigley, MD, The Methodist Hospital and Weill Cornell School of Medicine, and Prof. Purna Kashyap,… -
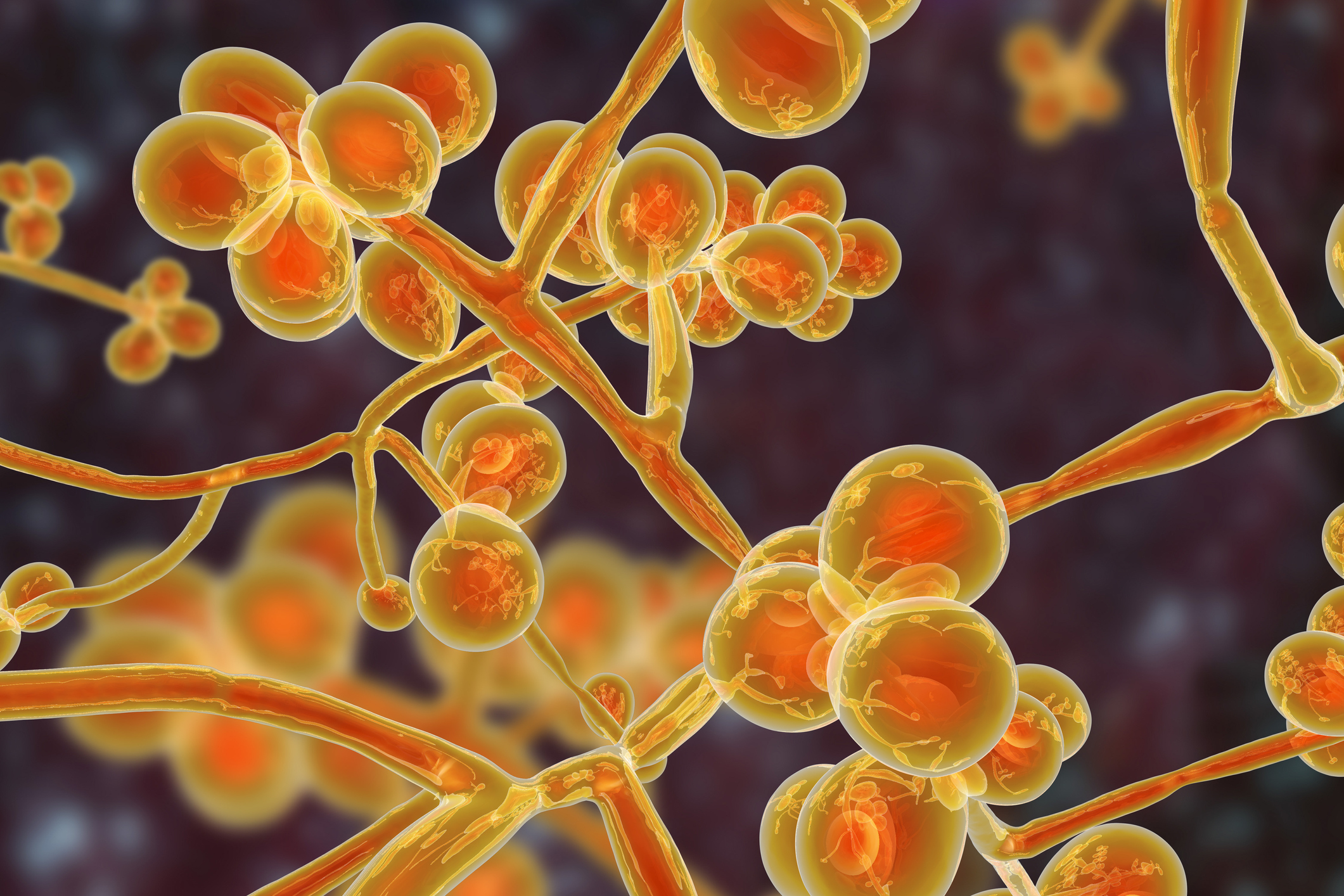
The Human Mycobiome: An ISAPP mini-symposium
ISAPP announces an open registration mini-symposium on the human mycobiome. Although the contribution of the intestinal microbiome in human physiology… -

ISAPP provides guidance on use of probiotics and prebiotics in time of COVID-19
By ISAPP board of directors Summary: No probiotics or prebiotics have been shown to prevent or treat COVID-19 or inhibit the… -

Connecting with the ISAPP community: Continuing to advance the science of probiotics and prebiotics
By Mary Ellen Sanders PhD, executive science officer, ISAPP On behalf of the ISAPP board of directors, I am reaching… -

Can probiotics and prebiotics go viral?
By Prof. Glenn Gibson, Food Microbial Sciences Unit, Department of Food and Nutritional Sciences, The University of Reading, UK I…