1-10 of 17 results
-
Insights into healthy aging: A story as told by gut microbiome (and other) metabolites
Metabolites, including those derived from the gut microbiome, offer a window into the complex biology of aging. They reflect not just how we live, but how well our bodies are adapting to the passage of time. -

Planning a Biotics Study? New Publication Recommends Adding Diet as a Variable
Both dietary patterns and specific foods are known to affect the digestive tract environment, either directly or indirectly (for example, by shaping the gut microbiome), and are therefore of interest as potential factors in the response of an individual to a biotic intervention. -
Can diet shape the effects of probiotics or prebiotics?
By Prof. Maria Marco PhD, University of California – Davis and Prof. Kevin Whelan PhD, King’s College London If you… -

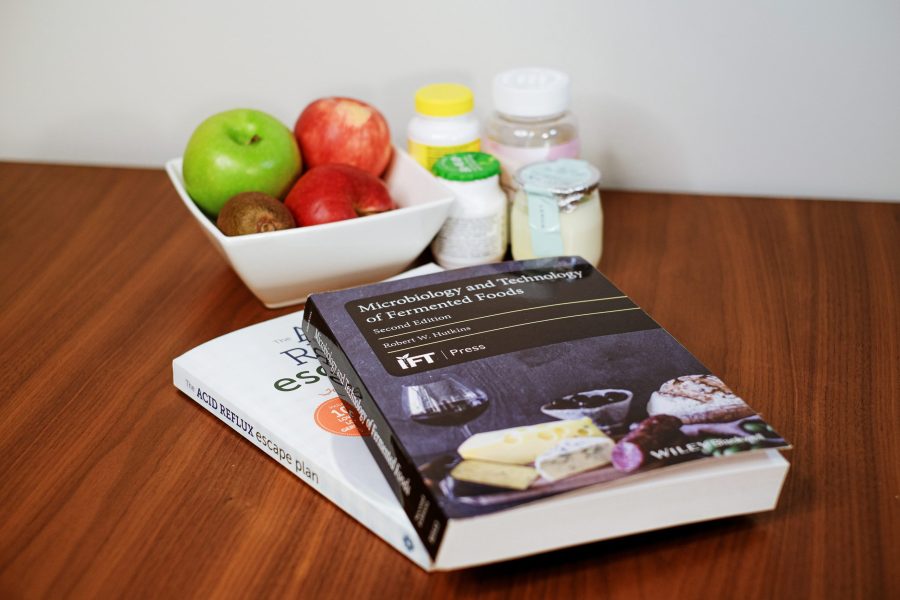
Episode 1: The science of fermented foods, part 1
The Science, Microbes & Health Podcast This podcast covers emerging topics and challenges in the science of probiotics, prebiotics, synbiotics,… -

New ISAPP Webinar: Fermented Foods and Health — Continuing Education Credit Available for Dietitians
Dietitians – along with many other nutritional professionals – often receive questions about consuming fermented foods for digestive health. But… -

Do fermented foods contain probiotics?
By Prof. Maria Marco, PhD, Department of Food Science & Technology, University of California, Davis We frequently hear that “fermented… -

Virtual events continue to fill gaps as in-person meetings are being planned
Prof. Bob Hutkins, PhD, University of Nebraska – Lincoln, USA For scientists, annual meetings provide coveted opportunities to hear about… -

Can fermented or probiotic foods with added sugars be part of a healthy diet?
By Dr. Chris Cifelli, Vice President of Nutrition Research, National Dairy Council, Rosemont IL, USA What about added sugar in… -

Ambient yogurts make a global impact
By Prof. Bob Hutkins, PhD, University of Nebraska Lincoln, USA Quick, which country consumes the most yogurt? Must be France?… -
New ISAPP-led paper calls for investigation of evidence for links between live dietary microbes and health
The past two decades have brought a massive increase in knowledge about the human gut microbiota and its links to…

